VisualEyes™ Support
Available Training
-
How to perform the Sinusoidal Harmonic Acceleration (SHA) test
-
How to perform the Velocity Step test
-
How to perform the Vestibulo-Ocular Reflex (VOR) Suppression test
-
How to use VisualEyes™ EyeSeeCam
-
How to perform the Dynamic Visual Acuity (DVA) test
-
How to perform the Advanced Dix-Hallpike test
-
How to perform the Supine Roll test
-
How to perform the Lempert (BBQ) Roll
-
How to perform the Gufoni Maneuver
-
How to perform the Epley Maneuver
-
How to perform the Dix-Hallpike test
-
How to perform the Brandt-Daroff Exercise
-
How to perform the Anterior Semont Maneuver
-
How to perform the Posterior Semont Maneuver
-
How to perform the Caloric test
-
How to perform the Optokinetic Nystagmus (OKN) test
-
How to perform the Gaze test
-
How to perform the Saccade test
-
How to perform the Spontaneous Nystagmus test
-
How to perform the Smooth Pursuit test
-
How to perform calibration procedures
-
How to perform the Lateral Head Roll test
-
How to perform the Subjective Visual Vertical (SVV) test
-
How to perform VORTEQ™ vHIT
-
How to perform Saccadometry
-
How to perform the Active Head Rotation test
-
How to perform the Ocular Counter Roll (OCR) test
-
How to use the Research Module
-
How to perform the Gaze Stabilization Test (GST)
-
How to perform Cervical Gaze testing
-
How to perform the Functional Vision Head Impulse Test (fvHIT™)
-
How to use keyboard shortcuts in VisualEyes™
-
How to perform Pupillometry
-
How to perform Self-Paced Saccades
-
How to perform the Smooth Pursuit Neck Torsion (SPNT) test
-
How to set up and troubleshoot monitors for oculomotor and optotype tests
How to perform Positional Nystagmus testing
What is positional nystagmus testing?
Positional nystagmus testing determines whether a change of position of the patient’s vestibular systems in space provokes nystagmus. Some nystagmus is only evident with changes in head position with respect to gravity. Both central and peripheral vestibular lesions can cause positional nystagmus and vertigo, and the examination focuses on distinguishing the two.
Most central positional nystagmus is static, in that the nystagmus persists as long as the head is kept in the provoking position. Nystagmus produced as a result of benign paroxysmal positional vertigo (BPPV), a peripheral vestibular pathology, is usually transient. Observations of the direction, latency and fatigability of nystagmus are important diagnostically.
Considerations
- Positional nystagmus is created by an asymmetry in the tonic resting rate of the two vestibular end organs.
- It is critical to identify the presence of spontaneous nystagmus prior to positional testing.
- There are many positions in which one might put the patient for examination. The positions described in this paper are considered standard procedure and provide the most diagnostic information.
- Positional testing is performed vision-denied (using covered VNG goggles) so that the patient does not have the means to suppress nystagmus.
- If the patient becomes strongly reactive when they are moved from one position to another, it is usually indicative of a vestibular lesion in the ear that is downward.
- If, within 15 seconds, no nystagmus is noted in the tracing, it is not necessary to continue the test. However, if nystagmus is noted, it is helpful to continue the recording for at least 30 seconds to watch for decay.
- Positional testing is also used in the diagnosis of benign paroxysmal positional vertigo (BPPV) of the lateral canal.
Patient instructions
“I am going to place goggles over your eyes. I will then assist you in moving into different positions. It is important to keep your eyes open at all times so that the cameras can record your eye movement. I will also ask you some questions to help keep you alert during the test.”
Description of positions tested
1. Neutral
Used to rule out spontaneous nystagmus. The patient is in the seated position on the table with vision denied.
2. Supine
The patient is lying on the table, vision denied, while his head is supported by the examiner and elevated at approximately 30º (the approximate position of the head relative to the body in its natural state).
3. Head Right/Head Left and Body Right/Body Left
Begin with the patient in the supine position described above. Gently guide the patient’s head to one side. Allow adequate time for nystagmus to occur (approximately 15 seconds). If no nystagmus occurs, return the patient’s head to the center, and then turn the patient’s head in the opposite direction and repeat procedure. If nystagmus is noted in either the head right or head left positions, immediately ask the patient to roll onto his shoulder toward the side of the affected ear.
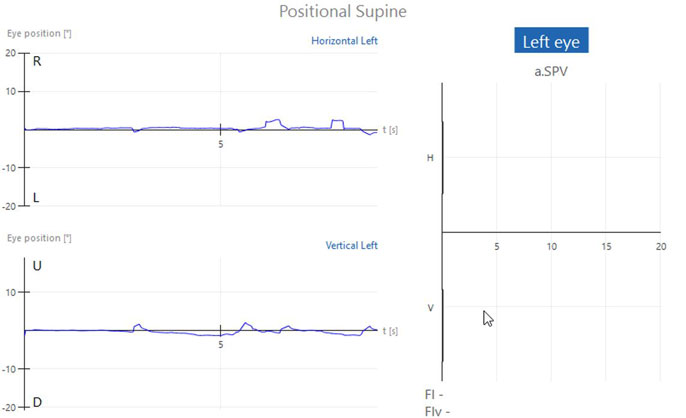
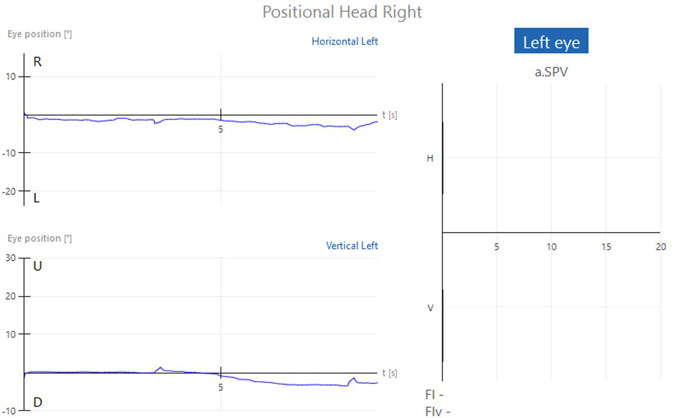
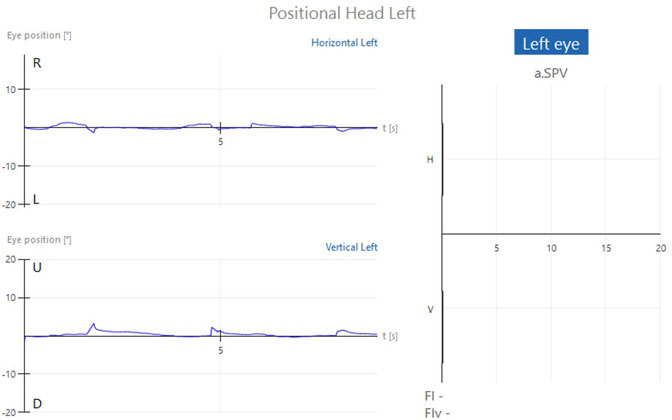
Normal positional testing results
If the patient does not have any form of positional nystagmus, the tracing will result in essentially a flat line for each position. The bar graphs for left and right beating nystagmus and down and up beating nystagmus will display as zero for all conditions (Figures 1a-c).
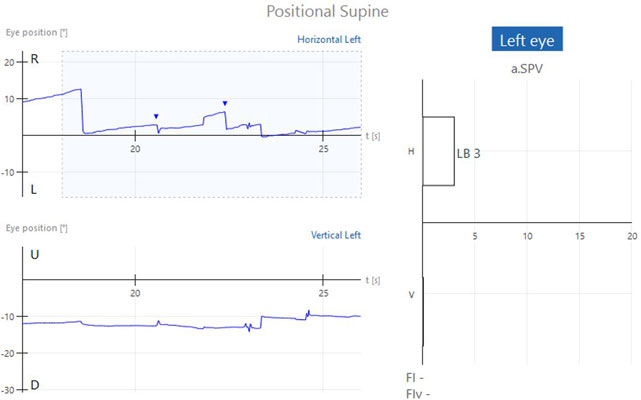
Abnormal positional testing results
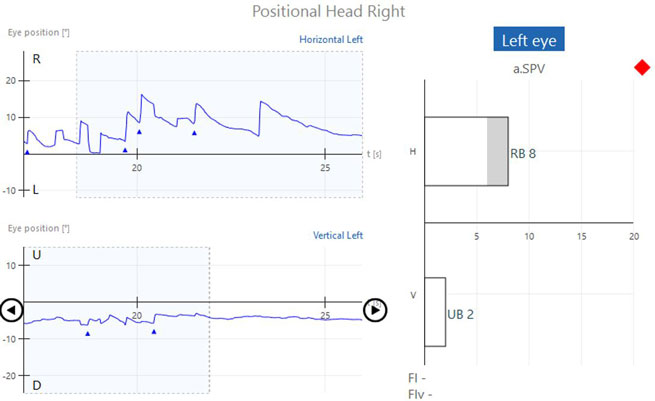
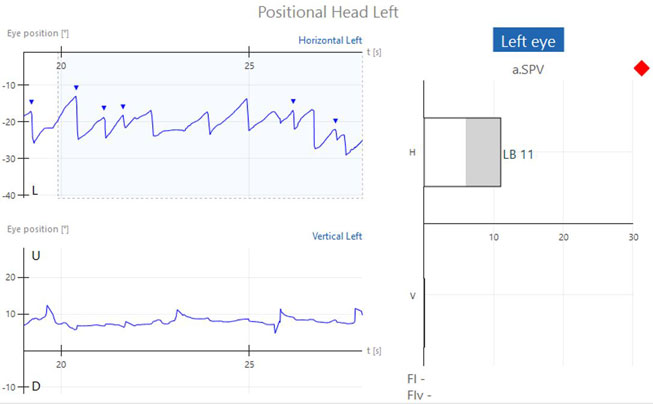
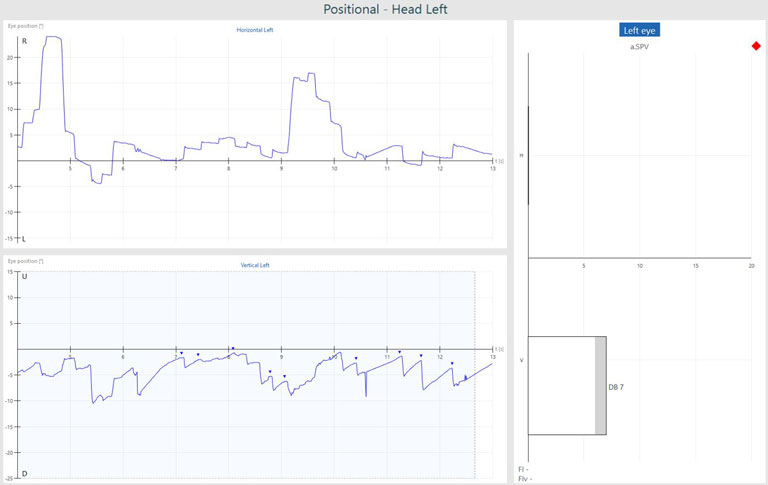
If positional nystagmus is present, nystagmus will be present in the horizontal and/or vertical channels. The nystagmus is represented by the triangles or green segments in the tracing and the averaged values for the strongest 10 seconds are shown in the bar graphs to the right of the tracing for each position (Figures 2a-c and 3).
Connection between type of nystagmus and site of lesion
Nystagmus that persists as long as the provoking position is maintained can occur with either central or peripheral vestibular lesions. Review of the waveforms is helpful. Pure downbeat nystagmus from central lesions is often accentuated in the reclining position, and sometimes may only be noted with this position. The lack of a torsional component differentiates this from anterior canal BPPV. Pure upbeat nystagmus can be positional. Positional torsional nystagmus has been reported with lateral medullary infarction.
Other features that indicate central disease are lack of latency, lack of fatigability, and the inability to suppress nystagmus with vision. Patients with static positional nystagmus without prior evidence of more typical BPPV should be investigated for central disease. Lesions of the cerebellar vermis are especially associated with static positional nystagmus.
Positional alcohol nystagmus
Alcohol can induce a static positional vertigo and horizontal nystagmus. Nystagmus beating towards the floor when the patient’s head is lying flat on its side emerges within 30 minutes of ingestion, peaking at 2 hours. As the blood alcohol level falls, 4 to 5 hours later, the nystagmus recurs in the opposite direction, and may last up to 12 hours. It is attributed to more rapid diffusion of alcohol into the cupula than the endolymph. The resulting difference in specific gravity temporarily imparts an abnormal sensitivity to linear acceleration, such as gravity.
References
For a complete discussion of positional testing and protocols, refer to:
Jacobson, GP, and Shepard, NT. Balance Functional Assessment and Management, 2nd Ed. San Diego; Plural Publishing, 2015
*NOTE: This is intended only as a guide, official diagnosis should be deferred to the patient’s physician.
