Subscribe to the Interacoustics Academy newsletter for updates and priority access to online events
Training in Functional Assessment and Rehab
-
Course: Advances in Vestibular Rehabilitation
-
Otolith Testing: Subjective Visual Vertical
-
The Benefits of Adding Functional Vestibular Assessments to Your Clinic
-
Otolith Testing in VNG
-
Diagnostic and Functional Evaluations of Vestibular Deficits in the Concussed Patient
-
Course: Objectifying the functional assessment of the dizzy patient
-
How to perform Dynamic Visual Acuity testing
-
Beyond bedside testing: Objective functional assessments of the Vestibulo-Ocular Reflex (VOR)
-
Gaze Stabilization Test in a case of concussion
-
Dynamic Visual Acuity (DVA) Test
-
The role of virtual reality in vestibular rehabilitation
-
Vestibular rehabilitation for concussion: A case study
-
Virtualis clinical education - Part 2
-
Virtualis clinical education - Part 1
-
Optimizing your functional balance assessment
-
Optimizing your vestibular rehabilitation programs
-
Motor Control Test (MCT)
-
Sensory Organization Test (SOT)
-
Rehabilitación vestibular: fundamentos para el abordaje integral de la persona con vértigo, mareo y desequilibrio
-
Evaluación y rehabilitación vestibular en la infancia
-
Computerized Dynamic Posturography (CDP): An Introduction
-
Limits of Stability (LOS)
-
Adaptation Test (ADT)
-
Getting started: Functional Vision Head Impulse Test
-
Modified Clinical Test of Sensory Integration on Balance CTSIB (mCTSIB)
-
Persistent Postural Perceptual Dizziness (PPPD) Unpacked: A Modern Approach to Chronic Dizziness
-
Functional Vision Head Impulse Test (fvHIT™)
-
From Diagnosis to Discharge: Utilizing the DATA model for comprehensive care of the dizzy patient
Clinical Test of Sensory Interaction on Balance (CTSIB)
Description
Table of contents
- What is the CTSIB?
- What does the CTSIB assess?
- Who should you assess with the CTSIB?
- Variations of the CTSIB procedure
- Clinical applications of the CTSIB assessment
What is the Clinical Test of Sensory Interaction on Balance (CTSIB)?
The CTSIB is a widely used clinical tool which was initially described in 1986 (Shumway-Cook and Horak, 1986) and later validated by Cohen et al. (2019), who demonstrated its utility in distinguishing individuals with vestibular disorders by comparing performance to neurologically typical adults. CTSIB evaluates the abilities of individuals to integrate visual, vestibular and somatosensory inputs to maintain balance, and laid the groundwork for development of further tools such as the Sensory Organization Test (SOT).
The central concept of the CTSIB is to systematically influence the visual, vestibular and somatosensory inputs involved in maintaining balance. The goal of this is to assist clinicians in identifying sensory deficits or issues of sensory integration which may be contributing to an individual’s postural instability.
The CTSIB assessment has been developed and refined over the years, with variations being proposed to enhance the clinical feasibility or utility of the original assessment. Despite the technological innovations such as dynamic posturography, variations of the CTSIB assessment continue to be widely utilized in the fields of physiotherapy, audiology and neurology to assess a patient’s sensory integration.
The insights gained from the CTSIB can go on to inform and shape personalized rehabilitation programs and act as an effective reassessment or outcome measure.
What does the CTSIB assess?
Unlike most of the animal kingdom, humans are unique in their preference to adopt an upright stance when walking or standing. Whilst upright posture does hold many advantages, it is an unstable stance which requires a complex system of sensory weighting and feedback loops to maintain stability. As touched on above, the primary sensory inputs responsible for balance in humans are listed in Table 1.
| Sensory input | Purpose |
| Vision | Provide information about our surroundings and current posture. |
| Vestibular | Provide information about head position or movement relative to gravity. |
| Somatosensory | Provide information about body positioning and weighting. |
Table 1: Sensory inputs responsible for balance in humans.
The ability of an individual to use these sensory inputs together to achieve a desired output to maintain or adjust balance is called sensory integration, which in this case refers to maintaining stable posture.
Sensory integration is a process which happens within the brain, arising from a range of complex connections and neural feedback loops, resulting in a range of reflexive and proactive balance responses to maintain stability.
The CTSIB therefore aims to provide not only an assessment of the sensory inputs, but also how these inputs are being integrated together to provide a functional output.
Who should you assess with the CTSIB?
CTSIB is a valuable tool for evaluating balance deficits across various populations. By systematically challenging sensory inputs, it helps clinicians identify the underlying causes of postural instability and tailor interventions accordingly (Cohen et al., 2019). Key groups who benefit from CTSIB are listed in Table 2.
| Patient type | Benefits of CTSIB |
| Patients with vestibular disorders | Assesses vestibular deficits and how patients compensate using visual and somatosensory inputs. |
| Older adults at risk of falls | Identifies sensory integration declines associated with aging to inform fall prevention strategies. |
| Neurological patients | Useful for conditions such as stroke, MS, Parkinson’s, and TBI to evaluate sensory processing and balance control. |
| Individuals with peripheral neuropathy | Determines reliance on visual and vestibular inputs due to impaired somatosensory function, common in diabetes. |
| Orthopedic injury patients | Tracks rehabilitation progress and adaptations in postural control after lower limb injuries or surgeries. |
| Athletes and high-performance individuals | Evaluates postural control post-concussion or injury, aiding return-to-play decisions and injury prevention. |
| Children with sensory processing disorders | Assesses sensory integration in pediatric populations with coordination or balance difficulties. |
Table 2: Patient populations that can benefit from the CTSIB assessment.
The CTSIB’s versatility makes it an essential tool in assessing balance control, guiding rehabilitation, and shaping individualized treatment plans for patients.
Variations of the CTSIB procedure
As discussed, since the assessment’s inception in 1986, there have been several variations to the CTSIB assessment. Below, we will describe and discuss the prevailing three approaches to the CTSIB, each of which provides us with progressively more diagnostic power.
Modified CTSIB (mCTSIB)
The bedside mCTSIB is the quickest and easiest variation of the CTSIB assessment to perform, consisting of only four test conditions and only requiring a foam balance pad to perform. Although performing the assessment is quick and easy, it is important to recognize the limitations of its ability to detect more subtle abnormalities due to its lack of objective postural assessment and limited control over the patient’s visual inputs.
To perform the mCTSIB, the patient is instructed to stand upright with their feet roughly shoulder-width apart and their arms crossed in front of their chest, or at their side. The patient’s goal for this assessment is to maintain this standing position for 30 seconds in each of the four test conditions. The four conditions of the mCTSIB are:
- Eyes open, firm surface
- Eyes closed, firm surface
- Eyes open, foam surface
- Eyes closed, foam surface
The primary measure for the mCTSIB is the number of seconds that the patient can hold the test position in each condition. The trial is considered over when any of the following occur:
- The patient opens their eyes (in conditions 2 and 4).
- The patient moves their arms from the test position to stabilize themselves.
- The patient requires manual assistance from the examiner to prevent a fall.
- The patient successfully maintains the test position for 30 seconds.
The patient has three attempts at each condition but can move on to the next condition straight away if they manage to maintain the position for 30 seconds.
Interpretation of the mCTSIB
When interpreting the bedside mCTSIB, the primary outcome of interest is which conditions the patient ‘failed’ by not successfully maintaining the test position for 30 seconds. Below are some of the common patterns of results you may find in clinic and what they could suggest.
Pattern one: Failure in eyes closed conditions (1 and 3)
| Firm surface | Foam surface | |
| Eyes open | Passed | Passed |
| Eyes closed | Failed | Failed |
Potential indication: Patient is ‘visually dependent’, or patient is not effectively using their vestibular/somatosensory inputs.
Pattern two: Failure in foam surface conditions (3 and 4)
| Firm surface | Foam surface | |
| Eyes open | Passed | Failed |
| Eyes closed | Passed | Failed |
Potential indication: Patient is not effectively integrating their visual and/or somatosensory inputs.
It is important to remember that the mCTSIB should only form one part of your overall assessment and further diagnostics are required to confirm any diagnosis.
Traditional CTSIB
The traditional bedside CTSIB consists of six conditions, with the addition of a ‘visual-conflict dome’ being used. The visual-conflict dome is intended to provide a secondary means to control the patient’s visual input to assess the impact upon their postural stability. The dome (photographed below) is a low-tech method to provide a patient with ‘sway-referenced’ vision.

Sway-referenced vision means that as a patient moves their head, what they are seeing visually will not change, as opposed to natural visual inputs which will move relative to the head movement. As a result, the difference between eyes closed and the visual-conflict dome is that eyes closed denies any input from the visual inputs, whereas the dome will result in a sensory mismatch, whereby the visual information being received has now become ‘unreliable’.
The procedure for the traditional bedside CTSIB is very similar to that of the bedside mCTSIB. The patient is instructed to stand upright with their feet roughly shoulder-width apart and their arms crossed in front of their chest, or at their side. The patient’s goal for this assessment is to maintain this standing position for 30 seconds in each of the six test conditions. The six conditions of the CTSIB are:
- Eyes open, firm surface
- Eyes closed, firm surface
- Visual conflict, firm surface
- Eyes open, foam surface
- Eyes closed, foam surface
- Visual conflict, foam surface
The primary outcome measure for the CTSIB is the number of seconds that the patient can hold the test position in each condition. It can also be beneficial to record the amount of sway demonstrated by the patient during each condition using the rating criteria of 1 = minimal; 2 = mild; 3 = moderate; 4 = fall.
The trial is considered over when any of the following occur:
- The patient opens their eyes (in conditions 2 and 4).
- The patient moves their arms from the test position to stabilize themselves.
- The patient requires manual assistance from the examiner to prevent a fall.
- The patient successfully maintains the test position for 30 seconds.
The patient has the attempts at each condition but can move on to the next condition straight away if they manage to maintain the position for 30 seconds.
Interpretation of the beside CTSIB
In healthy individuals with no history of postural instability or vestibular disorders, it is expected that they would be able to ‘pass’ all six conditions, with mild sway in the more challenging later trials.
Deviations from this expected pattern can indicate underlying sensory integration deficits. Below are common result patterns and their potential clinical implications.
Pattern one: Failure in eyes-closed and visual-conflict conditions (2, 3, 5, 6)
| Firm surface | Foam surface | |
| Eyes open | Passed | Passed |
| Eyes closed | Failed | Failed |
| Visual conflict | Failed | Failed |
Potential indication: The patient is visually dependent, relying heavily on vision for balance. This suggests difficulty integrating vestibular and somatosensory inputs.
Pattern two: Failure in foam surface conditions (4, 5, 6)
| Firm surface | Foam surface | |
| Eyes open | Passed | Failed |
| Eyes closed | Passed | Failed |
| Visual conflict | Passed | Failed |
Potential indication: The patient struggles to use somatosensory input effectively and may rely primarily on vision and vestibular input for stability. This pattern is common in individuals with peripheral neuropathy or postural instability.
Pattern three: Failure in visual-conflict conditions (3, 6)
| Firm surface | Foam surface | |
| Eyes open | Passed | Passed |
| Eyes closed | Passed | Passed |
| Visual conflict | Failed | Failed |
Potential indication: Failure in conditions 3 and 6 can suggest a visual preference.
Pattern four: Failure across multiple conditions, including firm surface (1, 2, 3, 4, 5, 6)
| Firm surface | Foam surface | |
| Eyes open | Failed | Failed |
| Eyes closed | Failed | Failed |
| Visual conflict | Failed | Failed |
Potential indication: Generalized balance impairment, which could be due to a neurological disorder, musculoskeletal weakness, or central integration deficits.
As with the mCTSIB, you should consider the results of the traditional CTSIB alongside other clinical findings. You may need to perform further assessments to confirm the presence of a specific sensory impairment and guide appropriate intervention strategies.
CTSIB using virtual reality and posturography
Advancements in technology have also led to advancements in the validity and accuracy of the CTSIB assessment procedure.
Virtual reality has given us far more advanced levels of control over a patient’s visual inputs than has previously been possible. By combining virtual reality with the enhanced level of objectivity and accuracy of posturography, the CTSIB VR takes the assessment to the next level of diagnostic power, providing greater opportunity for repeat accurate functional assessments of a patient’s balance.
The instrumented CTSIB VR consists of fundamentally the same six conditions as the traditional bedside CTSIB, being:
- Eyes open, firm surface
- Eyes closed, firm surface
- Sway-referenced vision, firm surface
- Eyes open, foam surface
- Eyes closed, foam surface
- Sway-referenced vision, foam surface
The most significant difference in testing technique with the CTSIB VR is the use of sway-referenced vision in-lieu of a visual-conflict dome. With the goggle attached firmly to the patient’s head, it is easy to achieve an arguably even better visual-conflict effect since the virtual reality goggle provides a visual stimulus which covers the patient’s full visual field.
The first significant addition to the CTSIB assessment to be introduced was posturography. Posturography is a method of objectively measuring a patient’s postural stability by recording a wide range of pressure readings from a pair of force plates. Posturography systems can be either ‘static’ or ‘dynamic’, with dynamic force plates having the extra ability to actuate in various directions, such as providing impulses for the Adaptation Test (ADT) or to aid in rehabilitative activities.
For CTSIB VR, no movement of the force plate is required, and you can therefore perform the assessment with either a StaticVR system or a MotionVR system with the force plates locked in place.
In the video below, Cassandra Anderson, PT, DPT demonstrates how to perform the CTSIB.
Compared to the mCTSIB or traditional CTSIB, CTSIB VR with posturography can be much more finely quantified, including accurate and detailed recordings of deviations in center of pressure (COP). This can show to us in a clear and easy way which of the conditions are the most challenging to the patient, and more importantly how their performance compares to age-matched normative data.
Reading a CTSIB VR report
Below you can see an example report from a CTSIB VR report. This was recorded using a MotionVR force plate and goggle combination, however you can perform the CTSIB VR using the StaticVR force plates to equally good effect. The system provides you with a range of data points which are calculated using the variations in pressure recordings made by the force plates.
Equilibrium and composite scores
The equilibrium score is represented as the average sway for each of the six conditions and is compared to age-matched normative data. In the objective data table below this, the sway velocity (degrees per second) is also listed. The composite score is a weighted average of sway for all the six conditions and is compared to an age-matched score.
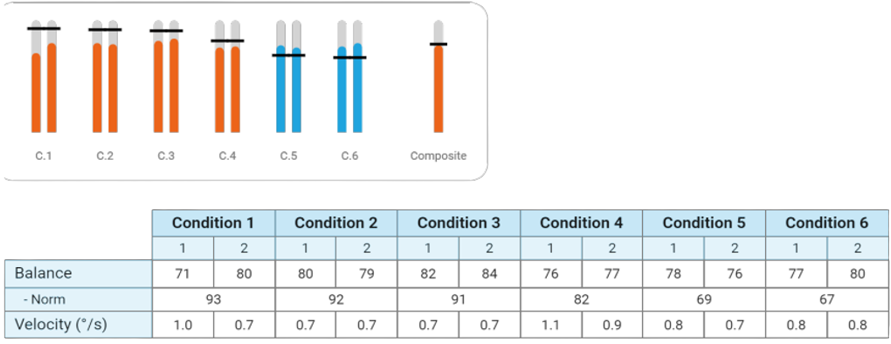
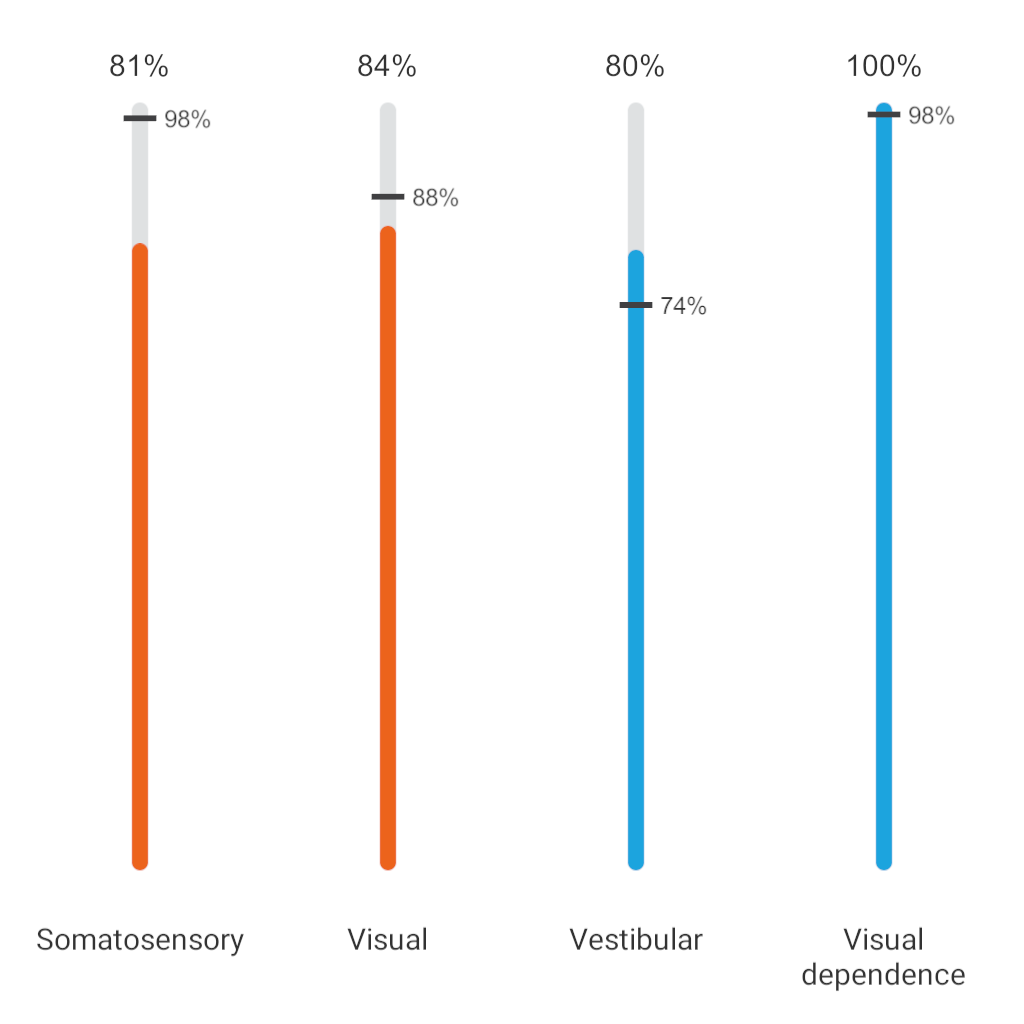
Sensory analysis ratios
Represented as average scores of specific conditions to identify functional impairments in the somatosensory, visual and/or vestibular systems, as well as to indicate if a patient has a visual preference (Figure 3).
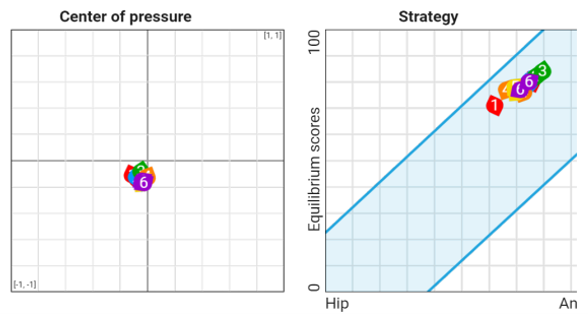
Center of pressure (COP)
COP is represented as the average COP for each condition. A perfect COP would be centered on the two lines in the graph below (Figure 4).
Balance strategy
Under dynamic conditions, the body is brought back to upright posture through certain movement strategies: ankle, hip or stepping. On the CTSIB VR, this is represented by a hip or ankle strategy based on the average equilibrium score of each condition.
Patients using an ankle strategy are represented as having a higher equilibrium score (numerically) as the ankle strategy has less overall sway to maintain posture / balance.
Clinical applications of the CTSIB assessment
The CTSIB assessment holds a diverse range of clinical applications in a range of and rehabilitative areas of practice. The data which you gather can provide you with a better insight into your patient’s function or challenges to help guide your further clinical decision making.
Let’s dive into some of the key applications below.
Diagnosis of sensory integration deficits
The CTSIB’s primary diagnostic purpose is to assess the quality of the integration of the sensory inputs and provide an indication of how well these are being integrated. See Table 3 for examples.
| CTSIB result | Possible indication |
| Failure in conditions where vision is removed (eyes closed). | Visual dependence or difficulty using vestibular/somatosensory inputs effectively. |
| Instability when standing on foam. | Somatosensory deficits, often seen in patients with peripheral neuropathy or proprioceptive dysfunction. |
| Struggles with visual-conflict or sway-referenced vision conditions. | Visual preference/dependency. |
Table 3: Using CTSIB results to assess sensory integration deficits.
Dynamic posturography studies reveal that CTSIB conditions isolating vestibular or somatosensory challenges – such as foam + eyes-closed – produce greater sway in vestibular-deficit patients, aligning with objective COP and sway velocity metrics (Julienne et al., 2024).
While the CTSIB assessment is often not enough to make a concrete diagnosis, identification of these more common patterns can help with not only producing an accurate diagnosis, but also:
Informing training and rehabilitation
When designing rehabilitation programs, we recommend adopting a ‘DATA’ driven approach (Figure 5).
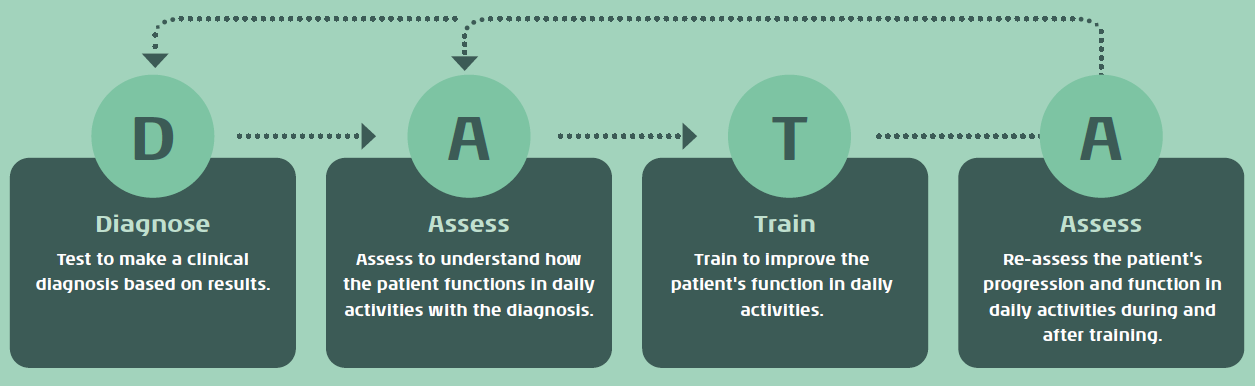
The CTSIB can fall into the ‘Assess’ and ‘(Re)Assess’ stages of this model to inform the rehabilitation activities prescribed to a patient. See Table 4 for examples.
| Indication from CTSIB | Possible rehabilitation strategy |
| Vestibular impairment | Vestibular rehabilitation therapy (VRT), focusing on gaze stabilization and habituation exercises. |
| Visual dependence | Therapy aimed at improving reliance on proprioceptive and vestibular inputs, such as balance training in reduced-vision conditions. |
| Somatosensory deficits | Targeted proprioceptive training, including unstable-surface exercises and tactile stimulation therapies. |
Table 4: Using CTSIB indications to inform rehabilitation strategies.
Fall risk assessment and prevention
Amongst patients with balance dysfunction and older adults, assessing for risk of falls is vital to support them in adopting safe, healthy and independent lifestyles. Poor performance in the CTSIB assessment can be an indicator that an individual may be at a higher risk of experiencing a fall and may inform interventions such as:
- Discussion and implementation of fall prevention strategies.
- Balance and strength training to target lower limb or core stability which in turn may lead to a reduction in falls risk.
- Environmental strategies such as informing appropriate footwear or assistive devices.
CTSIB, particularly in its virtual reality and posturography variations, allows for objective fall risk assessments, which may help clinicians to make more informed decisions on early intervention strategies.
Monitoring disease progression and treatment outcomes
For patients with progressive neurological conditions such as Parkinson’s disease, multiple sclerosis, or diabetic neuropathy, CTSIB provides a valuable method for tracking changes in balance function over time.
Regular CTSIB assessments can help clinicians determine whether a patient’s condition is stabilizing, deteriorating, or responding to treatment. Additionally, the use of objective posturography in the CTSIB VR allows for precise quantification of balance deficits, improving long-term monitoring and intervention planning.
Conclusion
Overall, the CTSIB assessment is quick to perform and is a useful addition in the clinical assessment of many disorders of balance and postural stability. The assessment can provide an insight into how patients are utilizing their vision, vestibular and somatosensory inputs to provide postural stability. You can assess a wide range of patient groups with the CTSIB, and multiple variations exist, each providing differing levels of diagnostic accuracy.
If you would like to learn more about the role of objective posturography in combination with virtual reality to assess patients, consider exploring our other articles:
- Adaptation Test (ADT)
- Limits of Stability (LOS)
- Motor Control Test (MCT)
- Sensory Organization Test (SOT)
- Computerized Dynamic Posturography (CDP)
References
Cohen, H. S., Mulavara, A. P., Stitz, J., Sangi-Haghpeykar, H., Williams, S. P., Peters, B. T., & Bloomberg, J. J. (2019). Screening for Vestibular Disorders Using the Modified Clinical Test of Sensory Interaction and Balance and Tandem Walking With Eyes Closed. Otology & neurotology : official publication of the American Otological Society, American Neurotology Society [and] European Academy of Otology and Neurotology, 40(5), 658–665.
Julienne, A., Verbecque, E., & Besnard, S. (2024). Normative data for instrumented posturography: a systematic review and meta-analysis. Frontiers in human neuroscience, 18, 1498107.
Khattar, V. S., & Hathiram, B. T. (2012). The clinical test for the sensory interaction of balance. International Journal of Otorhinolaryngology Clinics, 4(1), 41–45.
Shumway-Cook, A., & Horak, F. B. (1986). Assessing the influence of sensory interaction of balance. Suggestion from the field. Physical therapy, 66(10), 1548–1550.
Presenter

Get priority access to training
Sign up to the Interacoustics Academy newsletter to be the first to hear about our latest updates and get priority access to our online events.
By signing up, I accept to receive newsletter e-mails from Interacoustics. I can withdraw my consent at any time by using the ‘unsubscribe’-function included in each e-mail.
Click here and read our privacy notice, if you want to know more about how we treat and protect your personal data.
