Subscribe to the Interacoustics Academy newsletter for updates and priority access to online events
Training in Functional Assessment and Rehab
-
Course: Advances in Vestibular Rehabilitation
-
Otolith Testing: Subjective Visual Vertical
-
The Benefits of Adding Functional Vestibular Assessments to Your Clinic
-
Otolith Testing in VNG
-
Diagnostic and Functional Evaluations of Vestibular Deficits in the Concussed Patient
-
Course: Objectifying the functional assessment of the dizzy patient
-
How to perform Dynamic Visual Acuity testing
-
Beyond bedside testing: Objective functional assessments of the Vestibulo-Ocular Reflex (VOR)
-
Gaze Stabilization Test in a case of concussion
-
Dynamic Visual Acuity (DVA) Test
-
The role of virtual reality in vestibular rehabilitation
-
Vestibular rehabilitation for concussion: A case study
-
Virtualis clinical education - Part 2
-
Virtualis clinical education - Part 1
-
Optimizing your functional balance assessment
-
Optimizing your vestibular rehabilitation programs
-
Motor Control Test (MCT)
-
Sensory Organization Test (SOT)
-
Rehabilitación vestibular: fundamentos para el abordaje integral de la persona con vértigo, mareo y desequilibrio
-
Evaluación y rehabilitación vestibular en la infancia
-
Limits of Stability (LOS)
-
Adaptation Test (ADT)
-
Clinical Test of Sensory Interaction on Balance (CTSIB)
-
Getting started: Functional Vision Head Impulse Test
-
Modified Clinical Test of Sensory Integration on Balance CTSIB (mCTSIB)
-
Persistent Postural Perceptual Dizziness (PPPD) Unpacked: A Modern Approach to Chronic Dizziness
-
Functional Vision Head Impulse Test (fvHIT™)
-
From Diagnosis to Discharge: Utilizing the DATA model for comprehensive care of the dizzy patient
Computerized Dynamic Posturography (CDP): An Introduction
Description
Maintaining balance relies on a combination of both sensory inputs and motor outputs. In its most basic form, the three sensory inputs that contribute to this process come from the visual, vestibular, and somatosensory systems. The information from these inputs is integrated together in the brain to help determine an individual's body position and answer the question “where am I?”.
Following this assessment of body position, the brain sends signals to the motor system leading to decisions and choices on body movement to maintain stability and balance.
To assess an individual's balance function, it is important to investigate how well they can integrate sensory inputs as well as how well they can make corrective motor control outputs based on these sensory inputs.
Computerized Dynamic Posturography (CDP) provides clinicians with a tool to objectively assess these different systems and compare them against datasets of normally performing, aged-matched individuals.
Below, you can see an example of a CDP system: the Virtualis MotionVR solution. It comprises of a 360-degree dynamic posturography force plate, which measures the patient’s center of pressure and sway, along with a virtual reality headset allowing the clinician to replicate differing assessment and training environments.
Recent research indicates that 360-degree dynamic force plates can improve balance assessments in individuals that cannot stabilize with their medial/lateral ankle musculature (Wagner et al., 2023).

Which assessments can you perform on a CDP system?
CDP is an umbrella term that describes a series of assessments and training modules which you can use to rehabilitate the balance function of individuals with balance disorders.
The three dynamic assessments which form CDP are:
There are also other assessments you can perform, which don’t need the force plate to move but can still provide useful information on the patient’s ability to maintain balance. These are:
Lastly, you can use CDP systems to train patients with balance disorders. Following an assessment, you can use the CDP system alongside a virtual reality goggle to create individualized training programs, which are designed to improve balance function and allow patients with balance disorders to achieve their therapeutic goals.
We will now explore each of these subtests in more detail.
Sensory Organization Test (SOT)
The SOT informs clinicians on how well the patient integrates signals from the sensory system. It provides an assessment of the visual, vestibular, and somatosensory systems by providing an objective quantification of the impairments in each system.
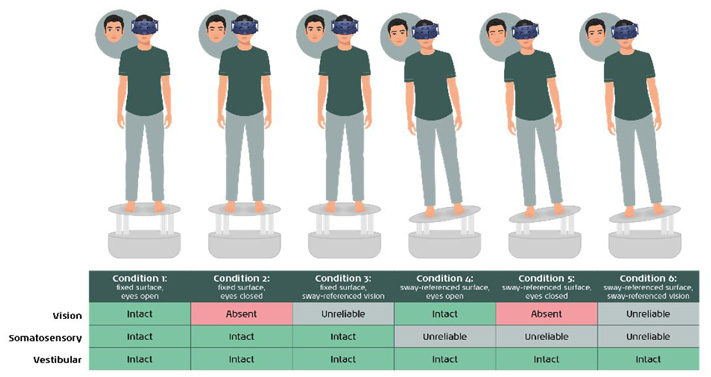
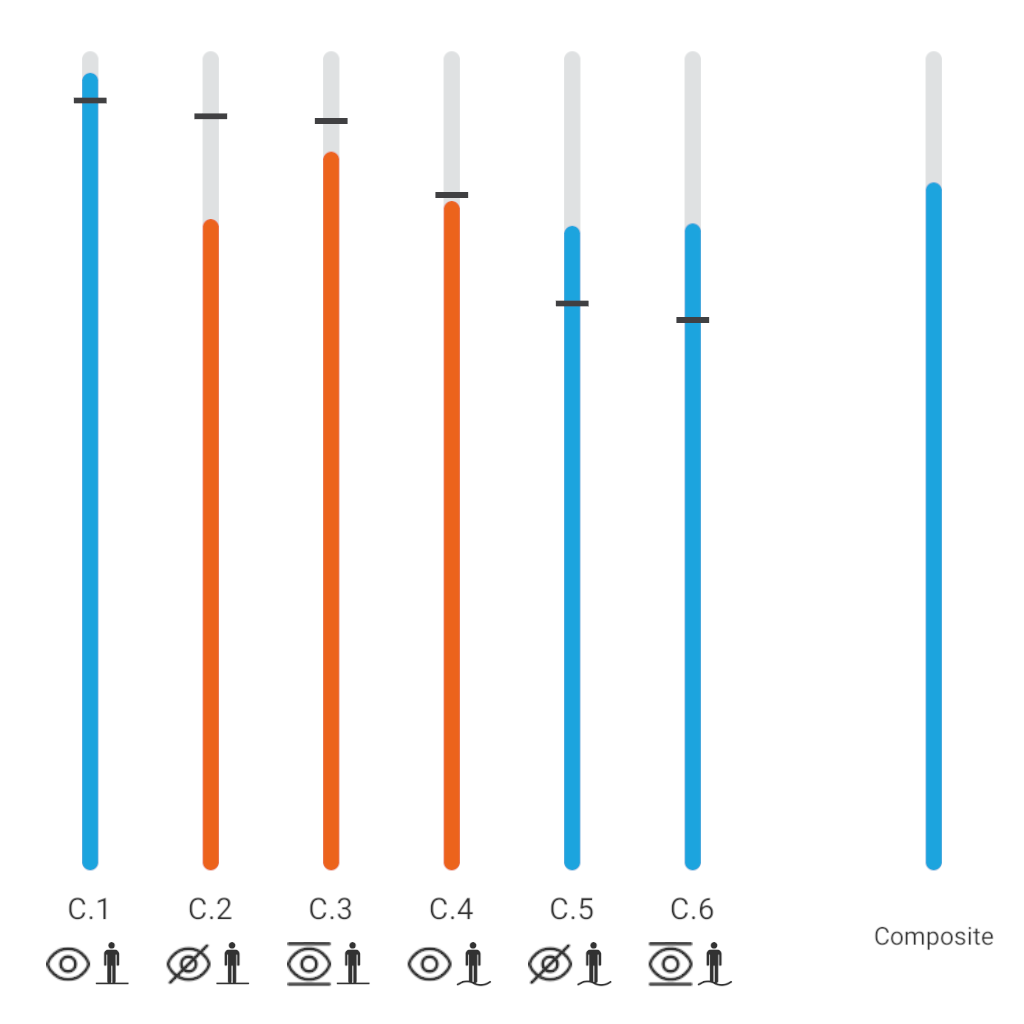
To complete an SOT assessment, the patient is exposed to six conditions which put each sensory system under differing levels of stress. These are standardized conditions and have a normative dataset which you can compare the patient’s performance to. Each condition either removes, reduces, or impairs one or more of the sensory inputs that the body uses to maintain its balance (Figure 2).
You can use the results from the SOT to guide yourself on where to focus training for best possible balance outcomes.
Read more: Sensory Organization Test (SOT)
Motor Control Test (MCT)
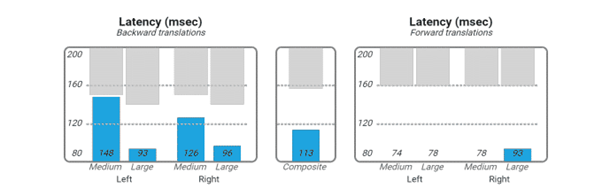
The MCT is designed to assess a patient’s automatic postural response to an unexpected movement. This is done by shifting the dynamic force plate in both forward and backward directions. The dynamic force plate analyzes and quantifies the patient’s responses to these movements and compares them against a set of normative data.
The results of the test provide an objective assessment of how a patient’s automatic postural control system is functioning. It can reveal if the brainstem and spinal cord are creating automatic responses in a coordinated pattern. It can also provide insights into the body’s strategy for responding to perturbations. This is essential knowledge when creating personalized rehabilitation programs.
Following the MCT, the postural control responses from the patient are extracted. A report is generated for latency, weight symmetry, and amplitude scaling. Below, you can see an example of latency, which refers to the duration it takes for the automatic postural response to initiate after the force plate begins to move.
Read more: Motor Control Test (MCT)
Adaptation Test (ADT)
A core function of the brain is to adapt to new experiences based on previous experiences. This is the hallmark mechanism which is measured during the ADT.
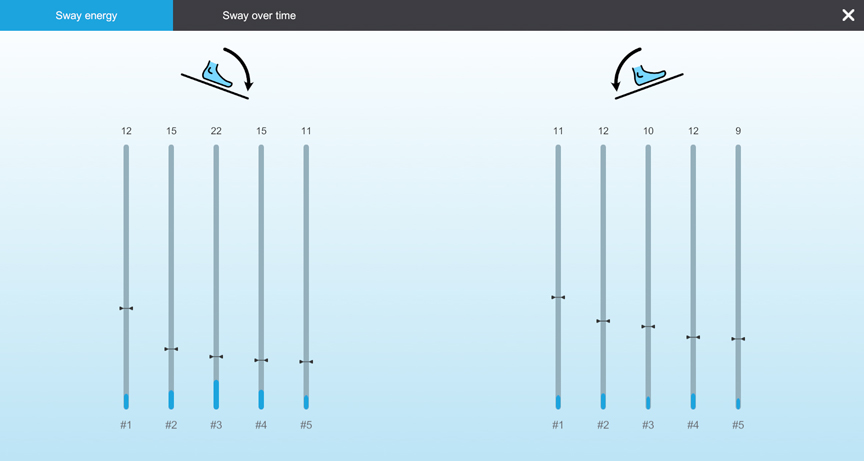
The ADT is designed to quantitatively assess a patient’s ability to react to the same unexpected movement over time. In normal balance control, we would expect the patient to improve their performance to repetitions of this movement due to this learning response from the central nervous system (Figure 4).
Knowing if someone can properly adapt to a stimulus is essential in creating training programs and therefore is an essential part of any CDP assessment.
Read more: Adaptation Test (ADT)
Limits of Stability (LOS)
The LOS assessment is designed to quantify the maximum excursion a patient can voluntarily lean their body to. It is performed in multiple directions. In normal balance control, we would expect the patient to be able to lean 4.5 degrees backward and 8 degrees forward, right and left (Figure 5).
Any patient with balance or functional deficits including instability or dizziness symptoms should have an LOS assessment performed. You can use the results to assess your patient’s fall risk. You can also use the LOS Rehab module (Figure 6) as part of postural control training where your patient works on increasing their LOS beyond what was measured in the assessment stage. This is most effectively done by combining the CDP system with a virtual reality headset.
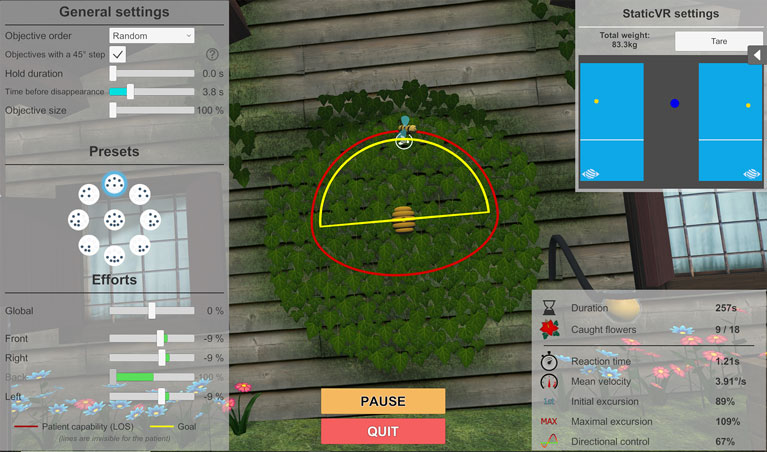
Read more: Limits of Stability (LOS)
Clinical Test of Sensory Interaction on Balance (CTSIB)
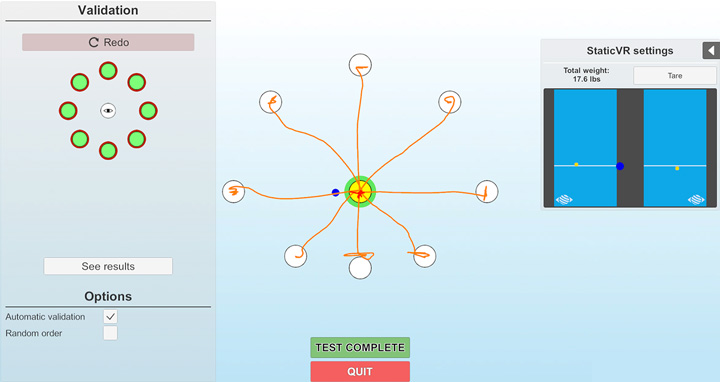
The Clinical Test of Sensory Interaction on Balance (CTSIB) is a widely used clinical tool which was initially described in 1986 (Shumway-Cook and Horak, 1986). CTSIB is designed to evaluate the abilities of individuals to integrate visual, vestibular and somatosensory inputs to maintain balance, and laid the groundwork for development of further tools such as the SOT.
To perform the CTSIB, the patient is instructed to stand upright with their feet roughly shoulder-width apart and their arms crossed in front of their chest, or at their side. The patient’s goal for this test is to maintain this standing position for 30 seconds in each of the test conditions.
The amount of test conditions depends on whether you’re performing the CTSIB or the modified CTSIB, also known as the mCTSIB or CTSIB-M (Table 1).
| Condition | mCTSIB | CTSIB / CTSIB VR |
| Eyes open, firm surface | Yes | Yes |
| Eyes closed, firm surface | Yes | Yes |
| Sway-referenced vision, firm surface | No | Yes |
| Eyes open, foam surface | Yes | Yes |
| Eyes closed, foam surface | Yes | Yes |
| Sway-referenced vision, foam surface | No | Yes |
Table 1: mCTSIB vs CTSIB conditions. Note that the mCTSIB does not include the conditions with sway-referenced vision.
With advancements in technology have also come advancements in the validity and accuracy of the CTSIB assessment procedure. Virtual reality has given us far more advanced levels of control over a patient’s visual inputs than has previously been possible. By combining virtual reality with the enhanced level of objectivity and accuracy of posturography, the Virtualis CTSIB takes the test to the next level of diagnostic power. This is called CTSIB VR.
The most significant difference in terms of the testing technique with CTSIB VR is the use of sway-referenced vision instead of a visual-conflict dome. With the goggle attached firmly to the patient’s head, it is easy to achieve the visual-conflict effect as the virtual reality goggle provides a visual stimulus which covers the patient’s full visual field.
You can see an example of Virtualis CTSIB results in Figure 7.
Read more: Clinical Test of Sensory Interaction on Balance (CTSIB)
CDP and balance training
Historically, CDP systems have been designed to provide an assessment of balance function and have had limited ability to perform balance training. However, when combined with virtual reality, you can use CDP for far more than assessing function. Training on the CDP system can come in many different formats with multiple training progressions, making it an incredibly powerful tool in balance rehabilitation.
Below is an example of the Sea Simulation Program, which simulates a scenario where the patient feels they are on a boat.
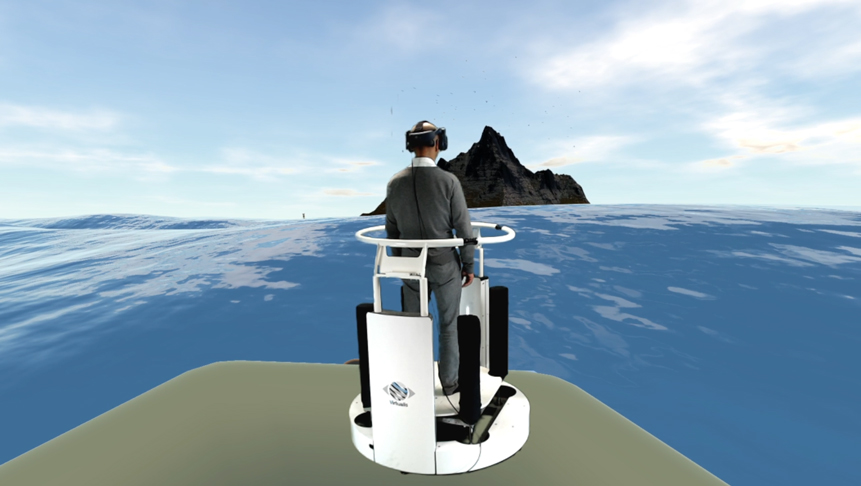
In this simulation, it is possible to change the characteristics of the sea, from being very calm to there being significant waves. The CDP system will move and mimic the visual representation of the wave. Here, we generate both a somatosensory response and a vestibular response from the movement of the CDP, and this is combined with the visual input received by the virtual reality headset.
By stimulating all three sensory inputs, we are better positioned as rehabilitation specialists to mimic real life stimulation with our patients and train all systems contributing to balance.
See Table 2 for other examples of training modules.
| Training module | Task |
| LOS Rehab | Rehabilitation of the patient’s stability limits, (ideally) based on LOS results. |
| Motion Program | Alter the settings of the MotionVR force plate by axis and amplitude, as well as its reaction speed and sensitivity, to create precise imbalance situations for rehabilitation purposes. |
| SkiVR | Immerses the patient in a ski-slope environment for lower-limb re-education and posturology. |
| BirdVR | Dual-task postural activity of the upper and lower limbs. The patient controls their center of gravity to navigate a bird through rings while catching butterflies with a net. |
Table 2: Examples of Virtualis training modules.
Conclusion
In conclusion, CDP is an evolving set of assessments and training modules which you can use in combination with virtual reality to better assess and treat patients with balance disorders.
It is unique in its ability to manipulate the level of sensory information we provide to our patients while at the same time objectively measuring their response to the manipulations.
CDP therefore provides the gold standard in both balance assessment and re-training.
References
Keshner, E. A., Mallinson, A. I., Longridge, N. S., Sinno, S., Petersen, H., & Perrin, P. (2023). Evolution of postural control assessment: From dynamic posturography to virtual reality. Frontiers in neurology, 13, 1054346.
Shumway-Cook, A., & Horak, F. B. (1986). Assessing the influence of sensory interaction of balance. Suggestion from the field. Physical therapy, 66(10), 1548–1550.
Wagner, A. R., Kobel, M. J., & Merfeld, D. M. (2023). Increased roll tilt thresholds are associated with subclinical postural instability in asymptomatic adults aged 21 to 84 years. Frontiers in aging neuroscience, 15, 1207711.
Presenter

Get priority access to training
Sign up to the Interacoustics Academy newsletter to be the first to hear about our latest updates and get priority access to our online events.
By signing up, I accept to receive newsletter e-mails from Interacoustics. I can withdraw my consent at any time by using the ‘unsubscribe’-function included in each e-mail.
Click here and read our privacy notice, if you want to know more about how we treat and protect your personal data.
