Subscribe to the Interacoustics Academy newsletter for updates and priority access to online events
Training in Functional Assessment and Rehab
-
Course: Advances in Vestibular Rehabilitation
-
Otolith Testing: Subjective Visual Vertical
-
The Benefits of Adding Functional Vestibular Assessments to Your Clinic
-
Otolith Testing in VNG
-
Diagnostic and Functional Evaluations of Vestibular Deficits in the Concussed Patient
-
Course: Objectifying the functional assessment of the dizzy patient
-
How to perform Dynamic Visual Acuity testing
-
Beyond bedside testing: Objective functional assessments of the Vestibulo-Ocular Reflex (VOR)
-
Gaze Stabilization Test in a case of concussion
-
Dynamic Visual Acuity (DVA) Test
-
The role of virtual reality in vestibular rehabilitation
-
Vestibular rehabilitation for concussion: A case study
-
Virtualis clinical education - Part 2
-
Virtualis clinical education - Part 1
-
Optimizing your functional balance assessment
-
Optimizing your vestibular rehabilitation programs
-
Motor Control Test (MCT)
-
Sensory Organization Test (SOT)
-
Rehabilitación vestibular: fundamentos para el abordaje integral de la persona con vértigo, mareo y desequilibrio
-
Evaluación y rehabilitación vestibular en la infancia
-
Computerized Dynamic Posturography (CDP): An Introduction
-
Limits of Stability (LOS)
-
Clinical Test of Sensory Interaction on Balance (CTSIB)
-
Getting started: Functional Vision Head Impulse Test
-
Modified Clinical Test of Sensory Integration on Balance CTSIB (mCTSIB)
-
Persistent Postural Perceptual Dizziness (PPPD) Unpacked: A Modern Approach to Chronic Dizziness
-
Functional Vision Head Impulse Test (fvHIT™)
-
From Diagnosis to Discharge: Utilizing the DATA model for comprehensive care of the dizzy patient
Adaptation Test (ADT)
Description
Table of contents
- What is the Adaptation Test (ADT)?
- What does the ADT assess?
- Who should you assess using the ADT?
- ADT procedure
- ADT results
- Clinical applications of the ADT
What is the Adaptation Test (ADT)?
The ADT is designed to quantitatively assess a patient’s ability to react to the same unexpected movement over time. In normal balance control, we would expect the patient to improve their performance over time due to a learning response from the central nervous system.
What does the ADT assess?
The ADT is one of the two motor assessments included in Computerized Dynamic Posturography (CDP), the other being the Motor Control Test (MCT). The ADT assesses the central sensory processing and motor output portions of the human balance system (Figure 1).
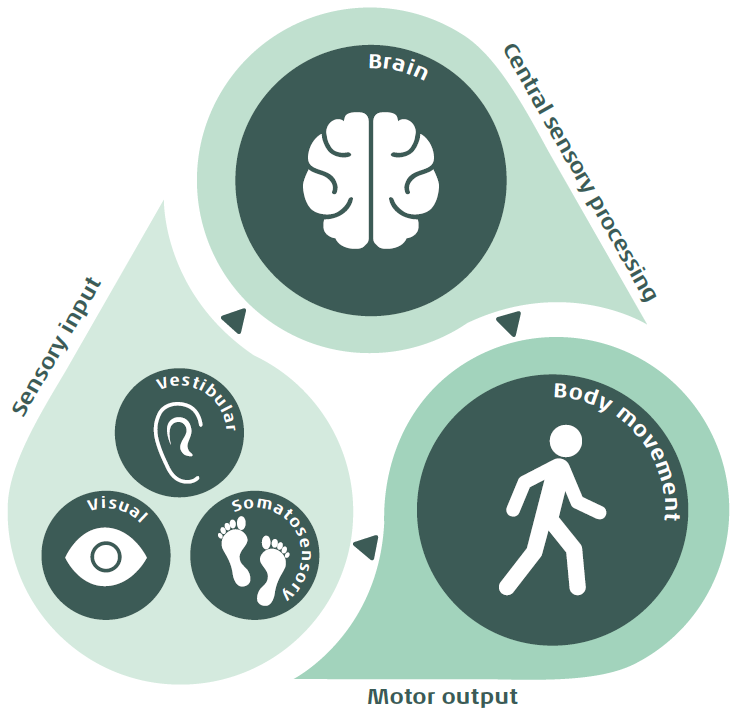
Central sensory processing
The ADT helps clinicians understand if the patient can adapt to a repeated stimulus over time, which is accomplished by central nervous system suppression (Reber et al., 2023). This is the hallmark mechanism for the ADT.
In normal balance control, the brain relies on prior experiences to interpret sensory information and adapt to new conditions. For example, when the body encounters an unexpected challenge to balance, such as slipping on ice, the brain finds a balance response from a similar previous experience to make a rapid postural adjustment.
These previous experiences help create internal models of postural control, allowing the central nervous system to predict responses, select appropriate motor responses, and improve balance strategies through practice and feedback. This process shows the importance of the brain’s plasticity to improve postural control.
Motor output
Another important part of the ADT is that it gives clinicians information on how the patient responds following an unexpected balance challenge, called a perturbation. In normal balance control, the patient should be able to both react quickly with a counter movement and maintain upright stability during a sudden change in force plate movement.
In contrast to the MCT, the ADT involves rotational rather than horizontal force plate movements. Due to this difference, reflexes measured during the ADT are not directly correlated with sway (Horak et al., 2016).
Instead, the ADT challenges the body’s postural control system to adapt to surface tilts by using more complex, long-loop automatic responses with central nervous system suppression, rather than simple, reflexive responses after linear movements.
Who should you assess using the ADT?
Like the other CDP assessments, you can use it with any patient with balance or functional deficits including instability or dizziness symptoms. Other important patient populations include people who fall or are at a high falls risk, elderly, or those with central nervous system diagnoses (Parkinson's disease, Multiple Sclerosis, etc.) (Jacobson et al., 1997). Patients must be able to stand still and unsupported for the assessment to be valid.
ADT procedure
The ADT consists of two different force plate rotational movements: toes up (ankle dorsiflexion) and toes down (ankle plantarflexion). The force plate rotates 8 degrees in 400 msec, resulting in an unexpected force plate rotation stimulus of 20 degrees per second in either direction. It traditionally consists of five trials in each direction with a pre-stimulus time of 0.4 seconds and a stimulus/response component of 2.0 seconds.
Typically, the assessment begins with a toes-up force plate rotational movement. These movements are completed at standard time intervals to measure the patient’s ability to adapt / use a learning effect.
Before testing, you should perform the following steps:
- Enter the patient’s age and height into the system for correct setup and comparison to normative data.
- Patients should have shoes removed (barefoot or in socks) to allow for standardized input of the somatosensory system.
- Center the patient's feet on the force plate. The front edge of the medial malleolus of each foot should be directly centered on the horizontal line of the force platform. The outer edge of the foot should be aligned with the antero-posterior line corresponding to the patient’s height (Figure 2).
- Assist patient with donning and fitting the VR headset for comfort.
- Patient’s arms at side of body (Figure 3).


Once the assessment begins, the force plate will first rotate five times in a backwards tilt direction, which results in a toes-up motion. A normal response would be for the patient to have an opposite but equal response at their ankles to maintain balance. The force plate position will reset between trials.
The force plate will then move five times in a forwards tilt direction, which results in a toes-down motion.
You can watch a video of the ADT being performed below.
ADT results
Following the ADT, the postural sway responses from all trials are extracted. A report is generated for sway energy and sway over time.
Sway energy
This is a calculation of velocity and acceleration produced by the patient during the initial two seconds following completion of the rotational stimulus. This is a measure of force and quantifies how well a patient can recover from the perturbation by minimizing anterior-posterior sway.
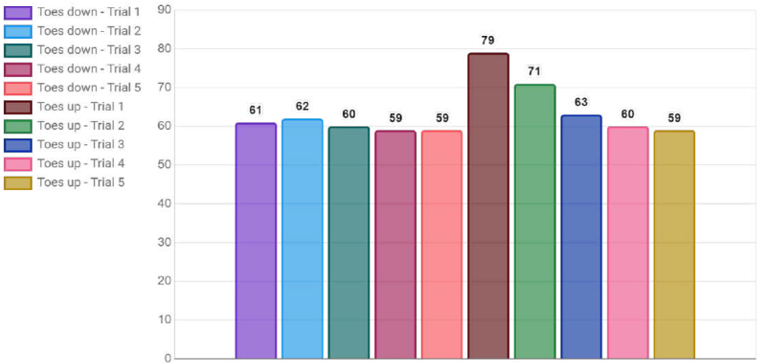
Normal central nervous system suppression should occur within five trials. Therefore, each successive response generated should be more efficient, leading to decreasing sway energy scores with each repetition.
For correct scoring, the patient must maintain stability through the assessment. If the patient loses their balance, steps or touches the support surface, you should stop and repeat the trial.
Normal sway energy
There are two categories of normal ADT results:
- An initial normal adaptive response followed by a flat line, indicating an effective initial strategy (shown in toes down trials in Figure 4).
- A progressive improvement over trials (shown in toes up trials in Figure 4).
Abnormal sway energy
There could be many abnormal ADT result patterns, some of which include:
- Falls on initial 1-2 trials then normal responses on final 3-4 trials. This pattern shows the patient does have a normal but delayed adaptive response. The clinician should consider behavioral / emotional factors.
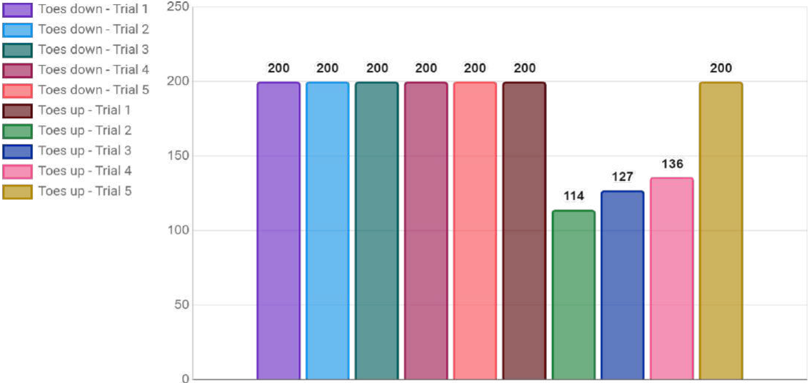
- Absent adaptive strategy shown by consistent falls in each trial (shown in toes down trials in Figure 5). The clinician should consider both musculoskeletal and central nervous system factors.
- Inefficient adaptive strategy shown with an increasing sway energy score over the trials (shown in toes up trials in Figure 5). The clinician should consider both musculoskeletal and central nervous system factors.
Sway over time
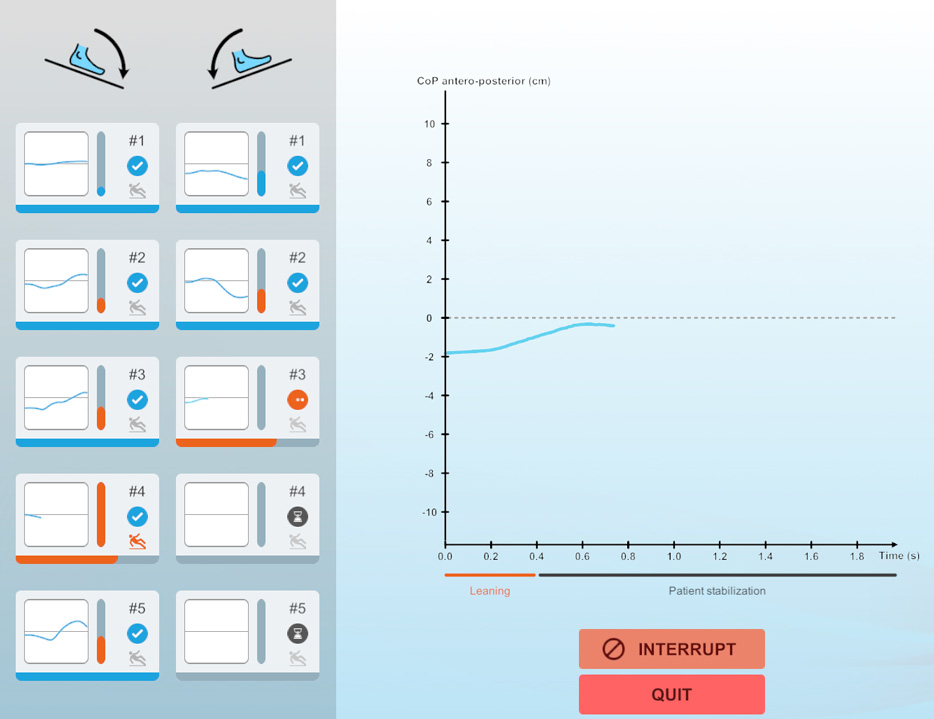
This graph plots the amount of center of pressure (COP) movement measured in centimeters (cm) along the ‘y’ axis over time along the ‘x’ axis. Time includes the duration of the pre-stimulus phase, the force plate movement itself, and the response period. You have the option of looking at single trials or a combination of all trials for both force plate movements.
It is recommended to review these graphs to ensure the correct movement is represented. For example, a toes down force plate movement should show an increasing negative sway energy value, which then shifts to an increasing positive value after the stimulus. This indicates the correct postural adjustment with a force in the opposite direction as the force plate movement (Figure 6).
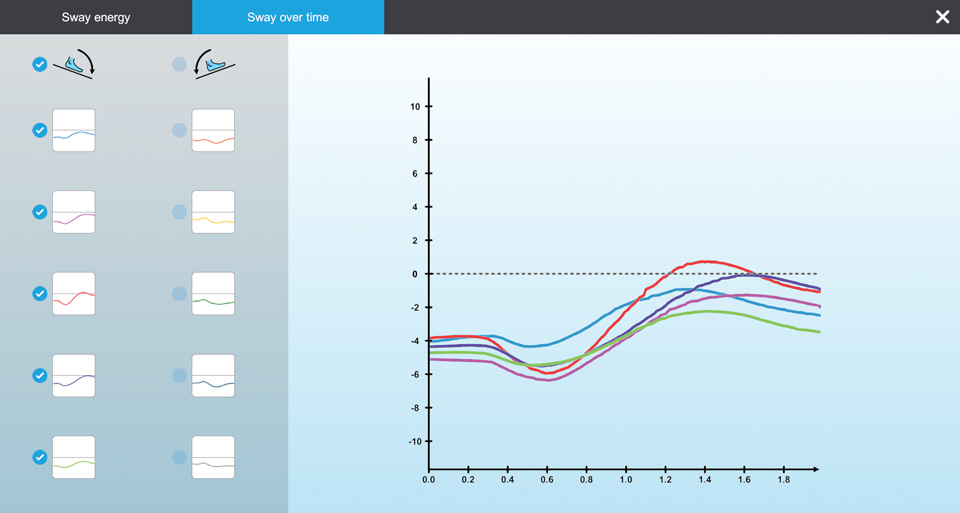
If this does not occur, repeat the trial to ensure correct analysis of end results. Below is an example of the real-time tracing option, which allows the clinician to verify that the graphing is correct.
Clinical applications of the ADT
The ADT is one assessment of the three Computerized Dynamic Posturography (CDP) assessments:
It is important to perform all three assessments for a comprehensive picture of your patient with balance dysfunction. Remember these assessments are not diagnostic but can help you decide if you need to refer for more testing.
Below are some clinical indications that you can take from the ADT assessment.
Falls risk
Patients may be at an increased risk of falls if they have abnormal results on the ADT. Common functional activities involve incline/decline surfaces with perturbations (like walking on a grassy hill).
It is important as a clinician to further assess possibilities for abnormal adaptive strategies and initiate appropriate referrals or rehabilitation plan of cares. Some examples are listed in Table 1.
| Deficit type | Example |
| Musculoskeletal | Range of motion, strength, pain |
| Central | Neurological or neurodegenerative disorders |
| Peripheral | Somatosensory/proprioceptive, vestibular dysfunction |
| Multi-factorial | Medical co-morbidities |
| Behavioral | Fear or anxiety |
Table 1: Deficits that can lead to abnormal adaptive balance strategies.
Functional responses
Abnormal and variable sway energy scores over the five trials could indicate a functional response. It is important to correlate ADT results with other assessment results, including variable amplitude scaling responses on the MCT, before assuming functional responses (Ortega-Robles et al., 2025).
Vestibular dysfunction
If the patient falls when the force plate is returning to the neutral starting position following the stimulus, the clinician should consider vestibular dysfunction. In normal balance, the vestibular system works to maintain postural stability during rotational movements occurring between two to eight degrees per second, which in the ADT correlates to the force plate speed returning to the starting position (Horak et al., 2016).
References
Horak, F. B., Kluzik, J., & Hlavacka, F. (2016). Velocity dependence of vestibular information for postural control on tilting surfaces. Journal of neurophysiology, 116(3), 1468–1479.
Jacobson, G. P., Newman, C. W., & Kartush, J. M. (1997). Handbook of balance function testing. Singular Publishing Group.
Ortega-Robles, E., Shalash, A., Ramírez-Bermúdez, J., & Arias-Carrión, O. (2025). Functional Movement Disorder: Evolving Mechanisms, Diagnostic Precision, and Personalized Multidisciplinary Care. Movement disorders clinical practice, 10.1002/mdc3.70136. Advance online publication.
Reber, T. P., Mackay, S., Bausch, M., Kehl, M. S., Borger, V., Surges, R., & Mormann, F. (2023). Single-neuron mechanisms of neural adaptation in the human temporal lobe. Nature communications, 14(1), 2496.
Presenter

Get priority access to training
Sign up to the Interacoustics Academy newsletter to be the first to hear about our latest updates and get priority access to our online events.
By signing up, I accept to receive newsletter e-mails from Interacoustics. I can withdraw my consent at any time by using the ‘unsubscribe’-function included in each e-mail.
Click here and read our privacy notice, if you want to know more about how we treat and protect your personal data.
