Subscribe to the Interacoustics Academy newsletter for updates and priority access to online events
Training in Functional Assessment and Rehab
-
Course: Advances in Vestibular Rehabilitation
-
Otolith Testing: Subjective Visual Vertical
-
The Benefits of Adding Functional Vestibular Assessments to Your Clinic
-
Otolith Testing in VNG
-
Diagnostic and Functional Evaluations of Vestibular Deficits in the Concussed Patient
-
Course: Objectifying the functional assessment of the dizzy patient
-
How to perform Dynamic Visual Acuity testing
-
Beyond bedside testing: Objective functional assessments of the Vestibulo-Ocular Reflex (VOR)
-
Gaze Stabilization Test in a case of concussion
-
Dynamic Visual Acuity (DVA) Test
-
The role of virtual reality in vestibular rehabilitation
-
Vestibular rehabilitation for concussion: A case study
-
Virtualis clinical education - Part 2
-
Virtualis clinical education - Part 1
-
Optimizing your functional balance assessment
-
Optimizing your vestibular rehabilitation programs
-
Motor Control Test (MCT)
-
Sensory Organization Test (SOT)
-
Rehabilitación vestibular: fundamentos para el abordaje integral de la persona con vértigo, mareo y desequilibrio
-
Evaluación y rehabilitación vestibular en la infancia
-
Computerized Dynamic Posturography (CDP): An Introduction
-
Adaptation Test (ADT)
-
Clinical Test of Sensory Interaction on Balance (CTSIB)
-
Getting started: Functional Vision Head Impulse Test
-
Modified Clinical Test of Sensory Integration on Balance CTSIB (mCTSIB)
-
Persistent Postural Perceptual Dizziness (PPPD) Unpacked: A Modern Approach to Chronic Dizziness
-
Functional Vision Head Impulse Test (fvHIT™)
-
From Diagnosis to Discharge: Utilizing the DATA model for comprehensive care of the dizzy patient
Limits of Stability (LOS)
Description
Balance is fundamental for daily activities, from walking and running to climbing stairs and reaching for objects. Maintaining stability and equilibrium is essential for postural control, helping prevent falls and injuries, especially in older adults and individuals with balance-related medical conditions.
Throughout human evolution, complex balance systems have developed to support our bipedal stance, which is the ability to stand on two limbs while maintaining our center of mass over a stable base of support. This postural control system relies on tonic muscle contractions acting against gravity, stabilizing body segments to maintain equilibrium (Sherrington, 1915).
Studies have shown that dynamic balance measures – such as the limits of stability assessment – remain consistent across multiple evaluations (Clark, 1997). Furthermore, center of pressure (COP) excursion, a key metric in the limits of stability assessment, has demonstrated high reliability and consistency in research (Juras, 2008).
Thus, assessing an individual's limits of stability is a crucial aspect of evaluating balance performance. In this article, we will take a deep dive into the limits of stability assessment, covering the following:
- What is the limits of stability assessment?
- Who should you assess the limits of stability on?
- Performing the limits of stability assessment
- Limits of stability results
- Clinical applications of the limits of stability assessment
- Five common reasons for limits of stability reduction
- Implications for the Sensory Organization Test (SOT)
What is the limits of stability assessment?
The limits of stability assessment is a crucial measurement of voluntary proactive movement control relative to a patient’s sway envelope and cone of stability. It quantifies the largest distance a person can lean their body without stepping, losing balance, or requiring external support.
Research (Tsang & Hui-Chan, 2003; 2004) has established theoretical limits of stability in healthy individuals (Table 1).
| Directional stability | Expected limits of stability |
| Anterior | 8 degrees |
| Posterior | 4.5 degrees |
| Lateral | 16 degrees (8 to each side) |
Table 1: Expected limits of stability in healthy individuals.
The center of gravity (COG) displacement, which is the extent to which an individual can lean without stepping or reaching for assistance, is measured objectively through a force plate that records COP values. Figure 1 illustrates how the COG shifts over the base of support (BOS) when standing upright.
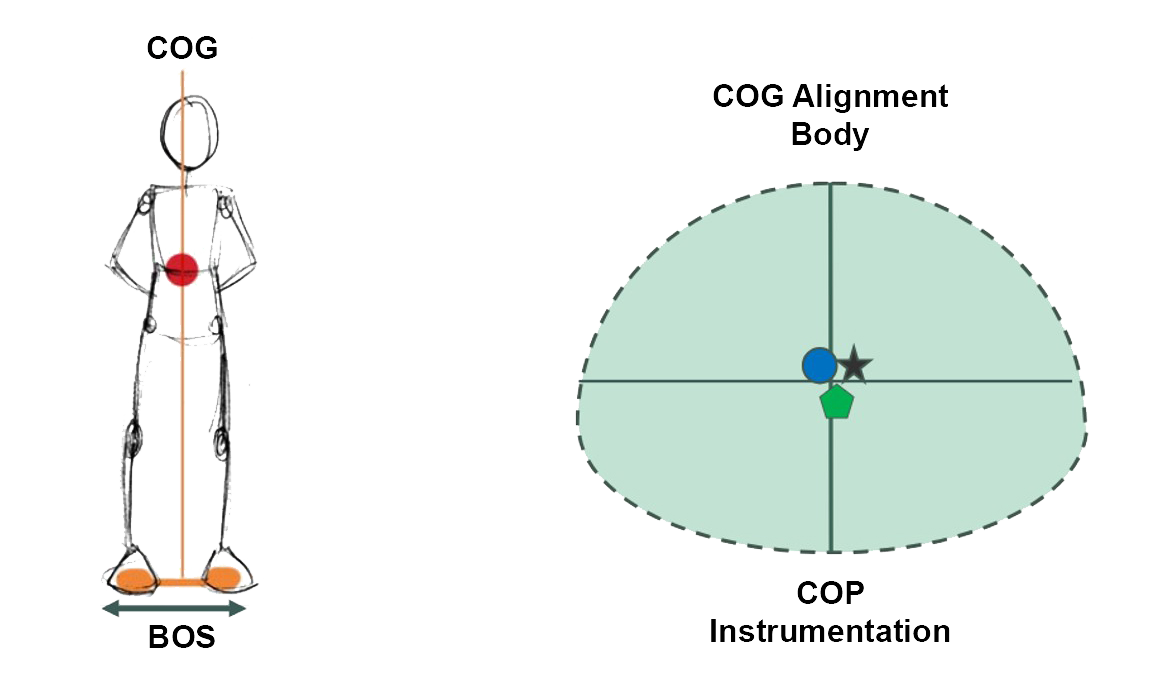
As discussed, the normal sway ‘envelope’ is illustrated in Figure 2. It has been evaluated over many years of research and is reported as 12.5 degrees anteroposterior and 16 degrees mediolaterally.
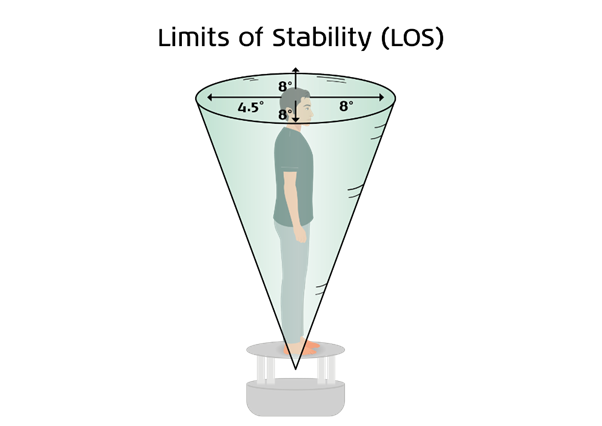
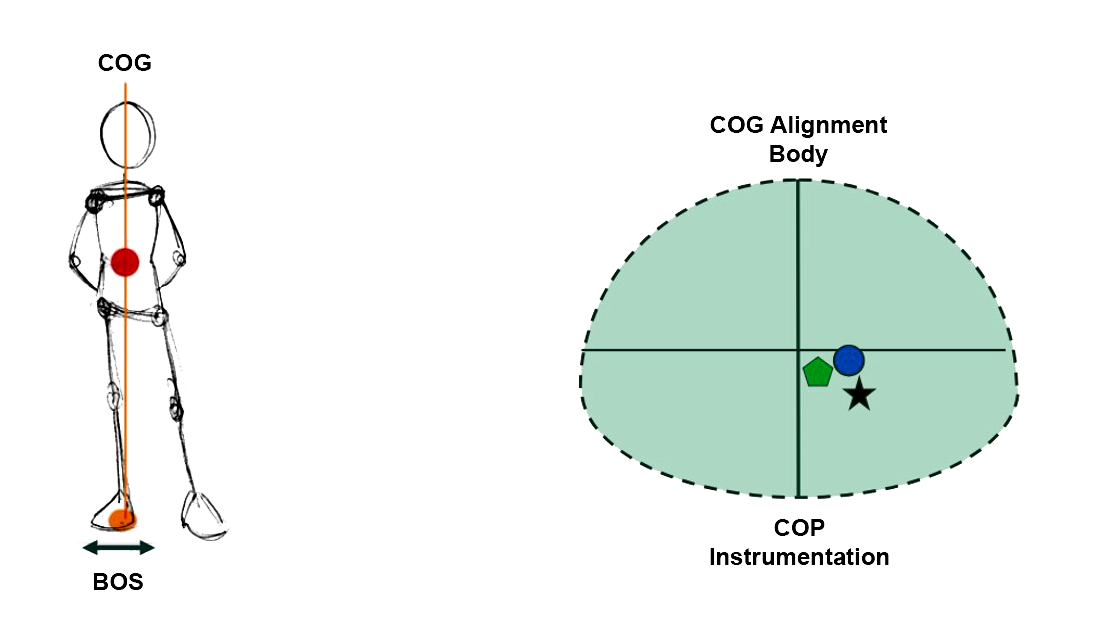
Figure 3 illustrates the change in COP measurement when the patient leans to the right and moves their COG over their BOS.
Who should you assess the limits of stability on?
The limits of stability assessment has been validated for use across multiple patient populations including geriatrics, community dwelling elderly, neurological disorders, and back and knee injuries.
It is reflective of biomechanical and neuromotor factors interacting together to allow for self-initiated movement in space as required for all functional activities and activities of daily living.
Performing the limits of stability assessment
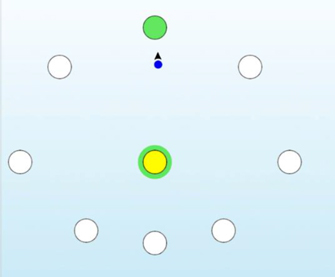
To perform the limits of stability assessment, the patient, standing on the force plate, must move their center of pressure by leaning successively towards a target, in the eight directions used for the assessment as shown in Figure 4.
This is typically performed in the clockwise direction, but you can also do it in the anticlockwise or random directions.
Instructions to the patient
For your convenience, please refer to the example script below:
“Keep the blue ball in the yellow center target. When the green circle appears [around the yellow target] hold still until the target circle turns green. Then move as quickly and accurately as you can towards the green target and hold it steady there.”
You can be certain your patient understands the task by practicing an adequate number of targets (at least one forward and one backward).
Performing the assessment
When the patient is ready to begin (with the blue ball in the center target), start the assessment to begin scoring Target Trial 1.
After the cue to move (blue ball), the patient should lean (ankle strategy) to move the cursor to the highlighted target with the green circle and hold it there if the green circle remains.
After eight seconds, the cursor will disappear. The patient should return to midline. The assessment is then advanced to the next target. Figure 5 illustrates a completed limits of stability assessment.
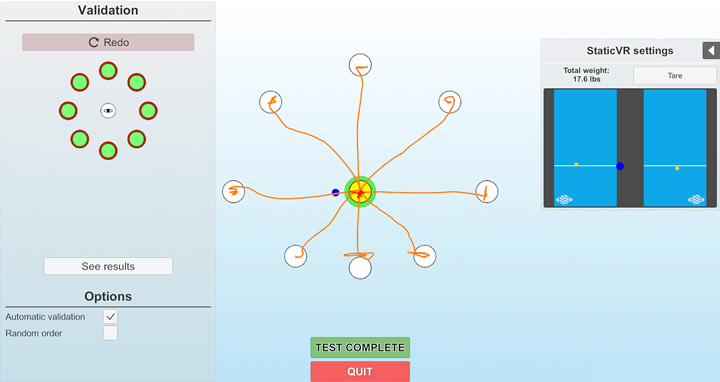
You should repeat the limits of stability assessment if your patient’s foot loses contact with the floor or if they switch from an ankle strategy, as the feet must remain in contact with the force plate during the assessment.
In the video below, Cassandra Anderson, PT, DPT demonstrates how to perform the limits of stability assessment.
Limits of stability results
Figure 6 illustrates an example of the full data set recorded during an limits of stability assessment.
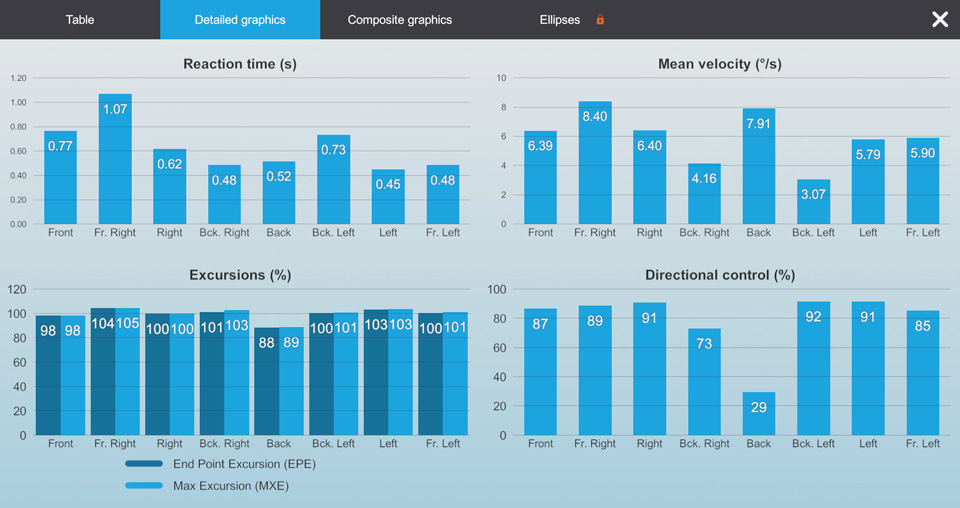
Let’s take a more detailed look at the data that is recorded during the assessment.
Movement time and velocity measures
The instructions to the patient are to move as quickly as possible (response) toward each limits of stability target when the green circle appears (stimulus). The reaction time and the movement velocity measures quantify the movement timing components of these self-initiated movements.
Reaction time
Reaction time is measured in seconds and reflects the onset of intentional patient movement toward the target as distinct from random movements while waiting for the cue (the green circle) to move.
This is calculated as the point in time at which the patient’s COG moves beyond the area occupied during the two seconds following the start of the trial but before the cue to move. Impairments in reaction time measures indicate delays in the patient’s ability to move on command or intention.

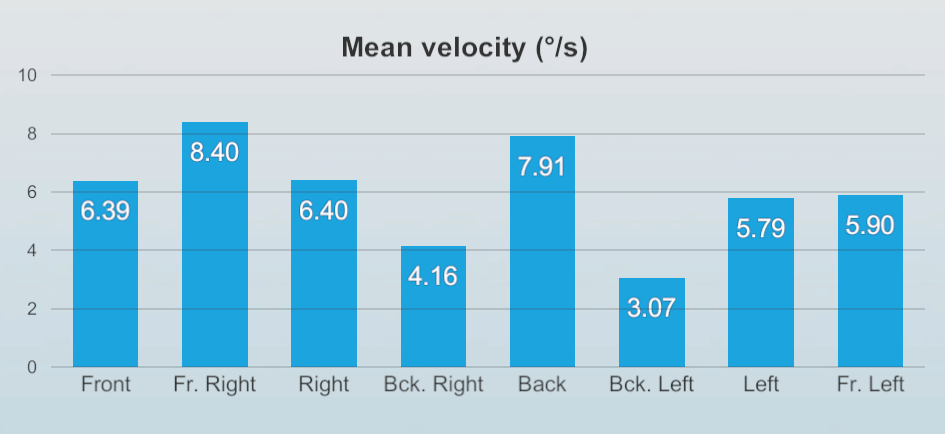
Movement velocity
This provides information on the average speed of the COG movement to the target in degrees per second. The movement velocity quantifies 5% to 95% of the distance from center to target, thus excluding acceleration and deceleration components in the calculation.
Excursion measures
The size or limits of self-initiated movements is reported relative to theoretical distances that normal individuals should be able to lean as described in Figure 2.
The end point excursion (EPE) and maximum excursion (MXE) measurements inform us how far an individual can shift their COG toward the theoretical limit (100%) in each of eight movement directions without loss of balance, falling, or taking a recovery step. It is a measure of the actual cone of stability or movement limit achieved by the patient during the limits of stability assessment.
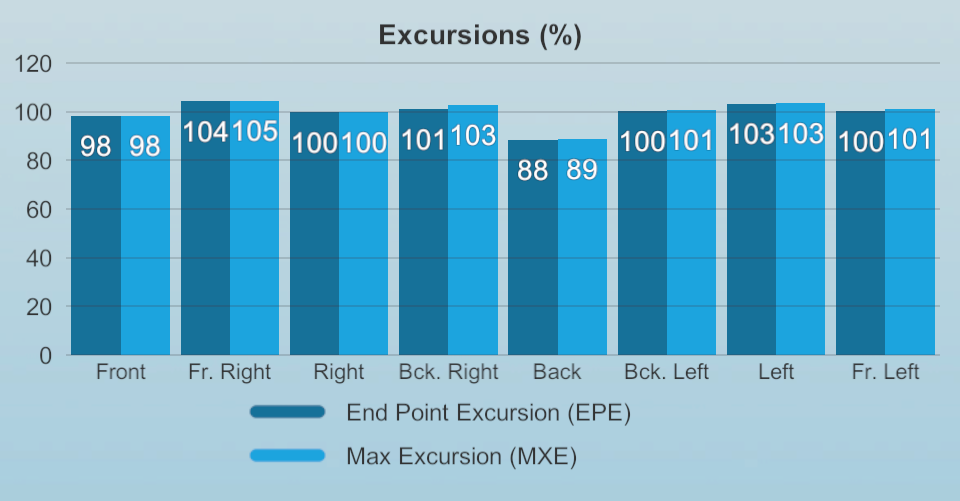
EPE provides a measure of how far the patient is willing to move on their first attempt shifting toward the target. A clinician might consider this suggestive of the individual’s perception of their own safety limits.
MXE indicates how far the patient finally moved their COG during the limits of stability assessment (Cheng et al 2004).
Both measures are compared to age-matched normative performance values. Individuals who achieve these values can be considered to have lower extremity range of motion, strength, and proprioception status within functional limits (Tsang & Hui-Chang, 2003; 2004).
Theoretically, the first (EPE) and final (MXE) attempt to move toward the target should be the same, or very close (EPE approximating MXE values). This is particularly true when movement precision and accuracy are the goal.
An EPE significantly less than MXE might indicate the presence of fear, anxiety, pain, or effort in that the patient may be self-restricting movement on their first attempt.
You should always correlate these impairment findings with their effect on function by relating them to appropriate functional balance measures.
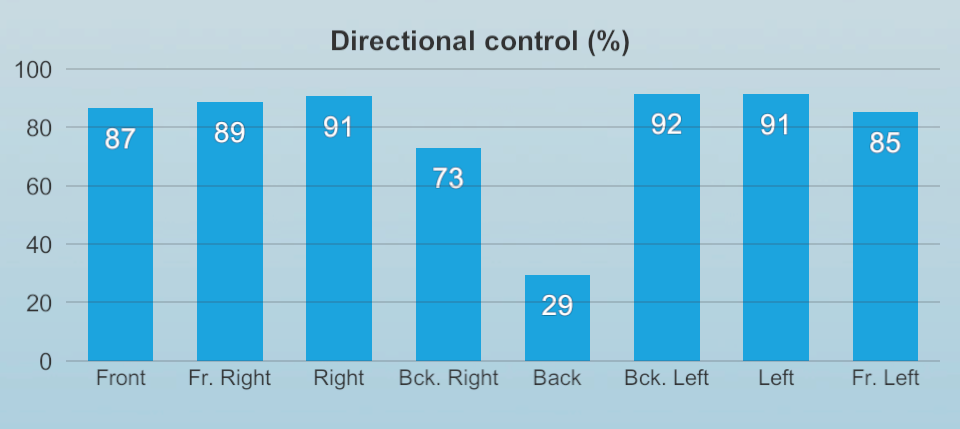
Directional control
The quality of movement control is quantified by directional control. This compares the amount of movement toward the target with the amount of movement away from the target, presented as a percentage (%).
Values can be interpreted as the percent accuracy of the self-initiated movement and are compared to age-matched normative performance values. Values approaching 100% indicate a straight path toward the intended target. Values below 100% indicate the amount of the distance that the individual is on the intended path.
Clinical applications of the limits of stability assessment
The limits of stability assessment is not a pathological localizing assessment; it represents the patient’s functional status. We can think of any impairment in the limits of stability as the patient’s response to a loss or abnormality at the body system level resulting from the presence of pathology(s) and/or maladaptation of the central nervous system to a health condition.
These limits of stability impairments can occur primary to the pathology but may also reflect secondary changes at locations distant to the pathology. Impairment level assessments of balance examine the effect of pathology upon body systems that include the (Jette, 2006):
- Sensory input (afferent) systems.
- Motor output and control (efferent) systems.
- Central nervous system (central integration or organization).
These impairments may:
- Warrant correlation with the medical examination findings.
- Re-direct the rehabilitation examination.
- Serve as a strong outcome measure for rehabilitation of specific underlying body system impairments.
Five common reasons for limits of stability reduction
Below, we will dive into five common reasons for limits of stability reduction.
1. Sensory and cognitive decline
Recent research highlights that postural skills in older adults depend on both biomechanical complexities and the sensory-attentional processing requirements of the task (Vermette et al., 2023). Aging often leads to reduced sensory reliability, which can impair automatic processing and the reweighting of visual, vestibular, and proprioceptive inputs. This shift increases controlled processing demands, elevating the cognitive-attentional load required for postural control (Goble et al., 2011; Henry & Baudry, 2019).
As cognitive function declines, postural control is significantly affected, resulting in narrower limits of stability and a heightened risk of falls. These effects become even more pronounced when individuals perform dual-task activities, where an added cognitive challenge further reduces balance efficiency.
2. Reduced neuromuscular control
The neuromuscular system plays a crucial role in postural control, particularly in coordinating muscular activity and joint torque, most notably at the ankle joint. Age-related or pathological changes in neuromuscular function may contribute to a reduction in limits of stability, affecting key balance parameters such as endpoint excursion, maximum excursion, and movement velocity.
Effective dynamic balance requires the ability to anticipate movement and adapt to both internal and external perturbations. This ability to produce precise and efficient postural adjustments is essential for maintaining stability during various activities (Vermette et al., 2023).
One critical parameter for assessing neuromuscular control is directional control, which provides insight into how well an individual can regulate movement accuracy and postural stability.
3. Reduce plantar flexor strength and lower limb conditions
Reduced plantar flexor muscle strength can significantly affect postural stability, leading to difficulties in supporting forward body lean. Additionally, limited ankle joint range of motion, the presence of pain, or lower limb pathologies can further impair balance performance, particularly influencing endpoint excursion and maximum excursion parameters (Melzer et al., 2008).
These factors contribute to decreased postural control, increasing the risk of instability and falls.
4. Fear of falling
Research indicates that fear of falling (FOF) is strongly linked to a reduction in limits of stability, particularly in forward-backward and left-right directional movements (Tomita et al., 2021). This fear is thought to decrease attentional resources available for balance control, making individuals more vulnerable to postural instability.
The effect is especially pronounced during dual-task activities, where cognitive demands further compromise balance, which is critical as most daily life activities require multitasking (Uemura et al., 2012).
Studies have consistently shown that individuals with heightened FOF experience increased reaction times and decreased movement velocity when performing the limits of stability protocol. This aligns with evidence suggesting that FOF alters sensorimotor processing, negatively impacting postural adjustment efficiency and increasing the risk of falls (Maki & McIlroy, 1997).
Moreover, FOF has been associated with reduced exploratory movement, further restricting an individual’s functional stability limits (Tinetti & Powell, 1993).
5. Proprioceptive and vestibular changes
Changes in proprioceptive and vestibular function are strongly linked to postural imbalance. When sensory input becomes unreliable for postural orientation, the time required to detect body position alterations and adjust through muscle activation is expected to increase (Henry & Baudry, 2019). This delay can significantly impair movement velocity and directional control, further compromising balance stability.
Additionally, environmental variations and dual-tasking conditions exacerbate difficulties in performing the limits of stability protocol. These factors challenge the body's ability to maintain equilibrium, making postural adjustments less efficient (Tomita et al., 2021; Vermette et al., 2023).
Implications for the Sensory Organization Test (SOT)
When interpreting Sensory Organization Test (SOT) results, it is essential to consider how reduced limits of stability can contribute to postural abnormalities (Nashner, 1989; 1990). A decrease in sway limits, defined as less than 12.5 degrees anterior-posterior and 16 degrees left-right, may result from several key factors:
- Ankle and foot muscle weakness or paresis.
- Orthopedic issues affecting the ankle and foot.
- Internal perceptual biases, causing resistance to larger postural displacements.
The interaction between limits of stability and sway amplitude in balance responses can manifest in two ways:
- Falls may occur even with minor increases in sway amplitude, particularly in patients with restricted stability limits.
- Raw balance data often indicates similar sway amplitudes between non-fall and fall trials in the moments leading up to loss of equilibrium.
Recognizing these influences is critical for refining SOT assessments and implementing targeted balance rehabilitation strategies.
References and further reading
Cheng, P. T., Wang, C. M., Chung, C. Y., & Chen, C. L. (2004). Effects of visual feedback rhythmic weight-shift training on hemiplegic stroke patients. Clinical rehabilitation, 18(7), 747–753.
Clark, S., Rose, D. J., & Fujimoto, K. (1997). Generalizability of the limits of stability test in the evaluation of dynamic balance among older adults. Archives of physical medicine and rehabilitation, 78(10), 1078–1084.
Clark, S., & Rose, D. J. (2001). Evaluation of dynamic balance among community-dwelling older adult fallers: a generalizability study of the limits of stability test. Archives of physical medicine and rehabilitation, 82(4), 468–474.
Goble, D. J., Coxon, J. P., Van Impe, A., Geurts, M., Doumas, M., Wenderoth, N., & Swinnen, S. P. (2011). Brain activity during ankle proprioceptive stimulation predicts balance performance in young and older adults. The Journal of neuroscience : the official journal of the Society for Neuroscience, 31(45), 16344–16352.
Henry, M., & Baudry, S. (2019). Age-related changes in leg proprioception: implications for postural control. Journal of neurophysiology, 122(2), 525–538.
Jette A. M. (2006). Toward a common language for function, disability, and health. Physical therapy, 86(5), 726–734.
Juras, G., Słomka, K., Fredyk, A., Sobota, G., & Bacik, B. (2008). Evaluation of the limits of stability (LOS) balance test. Journal of Human Kinetics, 19, 39–52.
Maki, B. E., & McIlroy, W. E. (1997). The role of limb movements in maintaining upright stance: the "change-in-support" strategy. Physical therapy, 77(5), 488–507.
Melzer, I., Benjuya, N., Kaplanski, J., & Alexander, N. (2009). Association between ankle muscle strength and limit of stability in older adults. Age and ageing, 38(1), 119–123.
Nashner, L. M. (1990). Sensory, neuromuscular, and biomechanical contributions to human balance. Paper presented at the APTA Forum on Balance, Nashville, TN.
Nashner, L. M., Shupert, C. L., Horak, F. B., & Black, F. O. (1989). Organization of posture controls: an analysis of sensory and mechanical constraints. Progress in brain research, 80, 411–397.
Sherrington, C. S. (1915). Postural activity of the muscle and nerve. Brain, 38(3), 191–234.
Tinetti, M. E., & Powell, L. (1993). Fear of falling and low self-efficacy: a case of dependence in elderly persons. Journal of gerontology, 48 Spec No, 35–38.
Tsang, W. W., & Hui-Chan, C. W. (2004). Effects of exercise on joint sense and balance in elderly men: Tai Chi versus golf. Medicine and science in sports and exercise, 36(4), 658–667.
Tsang, W. W., & Hui-Chan, C. W. (2003). Effects of tai chi on joint proprioception and stability limits in elderly subjects. Medicine and science in sports and exercise, 35(12), 1962–1971.
Tomita, H., Kuno, S., Kawaguchi, D., & Nojima, O. (2021). Limits of Stability and Functional Base of Support While Standing in Community-Dwelling Older Adults. Journal of motor behavior, 53(1), 83–91.
Uemura, K., Yamada, M., Nagai, K., Tanaka, B., Mori, S., & Ichihashi, N. (2012). Fear of falling is associated with prolonged anticipatory postural adjustment during gait initiation under dual-task conditions in older adults. Gait & posture, 35(2), 282–286.
Vermette, M. J., Prince, F., Bherer, L., & Messier, J. (2024). Concentrating to avoid falling: interaction between peripheral sensory and central attentional demands during a postural stability limit task in sedentary seniors. GeroScience, 46(1), 1181–1200.
Presenter

Get priority access to training
Sign up to the Interacoustics Academy newsletter to be the first to hear about our latest updates and get priority access to our online events.
By signing up, I accept to receive newsletter e-mails from Interacoustics. I can withdraw my consent at any time by using the ‘unsubscribe’-function included in each e-mail.
Click here and read our privacy notice, if you want to know more about how we treat and protect your personal data.
