Subscribe to the Interacoustics Academy newsletter for updates and priority access to online events
Training in VNG
-
Saccadometry in Clinical Practice
-
BSA Guidance for Eye Movement Recordings (2015)
-
BSA Guidance for Positioning Tests (2016)
-
Eye Movements with Progressive Supranuclear Palsy (PSP)
-
Cutoff for Normal vs Abnormal OCR Response
-
Significance of Upbeat Nystagmus in Smokers
-
How Large are Significant Square Wave Jerks?
-
Does Repositioning of Otoconia Affect Utricular Function?
-
How to Differentiate Between Spinocerebellar Ataxia Subtypes Using VNG
-
When is Torsional Nystagmus Significant?
-
Skew Deviation in HINTS Protocol: Next Step?
-
Course: Advances in Videonystagmography (VNG)
-
Course: Advances in BPPV
-
Course: Balance Testing for Beginners
-
Course: Balance Testing for Intermediates
-
What is the Optokinetic Nystagmus Test?
-
What is the Saccade Test?
-
BPPV: Case Studies
-
Benign Paroxysmal Positional Vertigo (BPPV): An Introduction
-
Otolith Testing: Subjective Visual Vertical
-
Otolith Testing: Ocular Counter Roll Test
-
Using the TRV Chair for BPPV Treatment
-
Physiology of the Otolith Organs
-
Diagnosing Central Vestibular Conditions with VNG
-
3D Eye Movement Recordings for BPPV Testing
-
Otolith Testing in VNG
-
The Importance of Vertical and Torsional Eye Movements in the Diagnosis of Vestibular and Neurological Conditions
-
VNG: Gaze Testing Without Fixation
-
VNG: Gaze Testing With Fixation
-
Oculomotor Testing: Theoretical Introduction
-
How to Diagnose Lateral Canal BPPV
-
Course: Saccadometry – a new tool for assessing central vestibular disorders
-
Course: Diagnosing Peripheral Vestibular Disorders
-
Course: The role of repositioning chairs in the diagnosis and treatment of BPPV
-
Course: Which test, when: Exploring optimal vestibular assessment protocol through illustrative case studies
-
Performing calibration for VNG testing
-
Performing spontaneous nystagmus testing (VNG)
-
Performing the gaze test (VNG)
-
Performing smooth pursuit testing (VNG)
-
Performing saccade testing (VNG)
-
Performing optokinetic testing (VNG)
-
Performing Dix Hallpike testing (VNG)
-
Performing positional testing (VNG)
-
Getting started: VNG
-
Understanding torsional eye movements
-
Interpreting the components of protocols that use torsional analysis in VisualEyes™
-
Interpreting the Dizziness Handicap Inventory (DHI) and VRBQ
-
Understanding Jerk Nystagmus
-
The role of eye movements in measuring brain function
-
BPPV: the importance of torsion and performing the manoeuvres accurately
-
Diagnostic driven rehabilitation strategies for concussion and other disorders
-
Physiology of torsional eye movements
-
Measuring torsional eye movements
-
The importance of measuring torsion
-
The role of audiology in concussion diagnostics
-
Eye movements in neuroperformance: A brain focused assessment of eye movements
-
Mise en route: VNG
-
Beyond the basics: Identifying and minimizing artifacts in VNG
-
VPPB: Una Introducción
-
Vidéonystagmographie (VNG) : une introduction
-
Effectuer un test de saccade (VNG)
-
Effectuer le test optocinétique (VNG)
-
Effectuer un test Dix Hallpike (VNG)
-
Effectuer un étalonnage pour les tests VNG
-
Effectuer des tests de position (VNG)
-
Effectuer un test de nystagmus spontané (VNG)
-
Effectuer un test du regard (VNG)
-
Effectuer des tests de poursuite lente (VNG)
-
VNG pruebas oculomotoras
-
Erste Schritte: Video-Nystagmographie (VNG)
-
Kalibration der Augenpositionen
-
Einführung VNG
-
Blickrichtung / Blickstabilisierung Test
-
Spontan Nystagmus
-
Saccaden Test
-
Glatte Blickfolge Test
-
Optokinetik Test
-
Lage-/Lagerungstest
-
Dix-Hallpike Test
-
Kalorik-Test
Understanding the Smooth Pursuit Neck Torsion (SPNT) test
Description
Authored by Liz Fuemmeler, Au.D. and reviewed by Michelle Petrak, Ph.D., and Daniel Demian, DC.
Table of contents
- Oculomotor performance in daily life
- What is the Smooth Pursuit Neck Torsion (SPNT) test?
- How the SPNT test works
- SPNT difference (SPNTdiff)
- Interpreting results
- Significance of the SPNT test
Oculomotor performance in daily life
Normal oculomotor performance is critical for being able to function in daily life (Table 1).
| Task | Example |
| Track objects as they move (pursuit) | Following a car as it drives away |
| Quickly change focus from one item to another (saccade) | Looking from side to side on a computer screen |
| Hold gaze on an object of interest (gaze) | Looking at a stoplight and waiting for it to change |
Table 1: Examples of how normal oculomotor performance helps us to function in daily life.
We recognize the importance and necessity of these oculomotor functions and test for them routinely in the videonystagmography (VNG) test.
However, in the VNG, we tend to only assess these oculomotor tests in a neck neutral position, meaning that the patient’s head and body are directly facing the stimulus. While this can give us an insight into the physiological ability of the oculomotor pathways, it doesn’t always represent functional abilities of the patient in their daily lives.
How often are you using your eyes only in a neck neutral position in daily life? Are you reading this article with your head and body perfectly facing the computer or phone screen? In our daily lives, we use our eyes (oculomotor system) with our head turned all the time. So why have we not been testing for this in the clinic?
That is why we have added the Smooth Pursuit Neck Torsion (SPNT) test in VisualEyes™ 3.2.
What is the SPNT test?
The SPNT test allows for comparison of oculomotor movements in neck neutral versus neck turned conditions. The purpose of this test is to determine if and how much the neck is contributing to abnormal oculomotor performance.
This is not a new test in literature. The SPNT test was first introduced in 1998 by Tjell and Rosenhall [1] to screen deficiencies in eye movement because of altered afferent input from the cervical spine. This test and the measurement parameters (SPNT difference, discussed below) have been shown to be a repeatable and reliable assessment to use in the clinic [2].
Different head and body positions are also not new to VNG. Especially during positional and positioning testing, we have several assessments where the patient’s head is not in a neck neutral state.
For example, we test for the present of nystagmus in head right and head left conditions while laying supine. If we observe nystagmus in one of these conditions, we test for body right and body left conditions to see if the neck is contributing to the observed nystagmus.
Similarly, the SPNT test allows us to see if the neck is contributing to abnormal oculomotor performance – this time in a seated position, not supine.
How the SPNT test works
The SPNT test involves three subtests:
- Horizontal smooth pursuit (neck neutral)
- Horizontal body right (neck torsion)
- Horizontal body left (neck torsion)
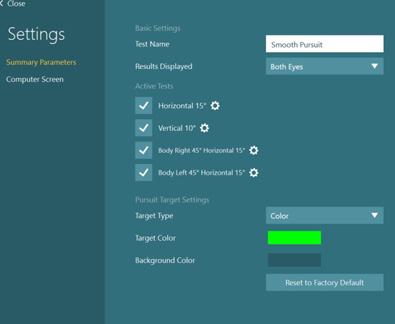
Horizontal smooth pursuit
First, you perform the test in a neck neutral condition (normal horizontal smooth pursuit). This is typical pursuit testing that we are familiar with in our VNG battery. From this test, we get a gain value that informs us how closely the patient’s eyes followed the target at different frequencies or speeds. 100% gain indicates the patient followed the pursuit moving target perfectly.
Horizontal body right and left
The next set of tests are the body right and body left positions with the body turned to 45 degrees in each direction and the head turned back to 0 degrees. This degree of neck torsion has been shown to be most effective for assessment [3].
We perform these tests to see if the neck is playing a role in oculomotor dysfunction. Complete the same pursuit test with the patient turned 45 degrees to the right or to the left.
Tip: Keep in mind that body right means that the neck is being turned to the left (Figure 2). Therefore, if someone had left sided neck concerns, their pursuit results on the body right subtest would likely be affected.

You should perform three subtests at the same frequencies (.1 to .5 Hz) for the comparison (read below) to be equivalent.
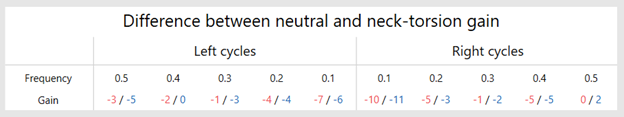
SPNT difference (SPNTdiff)
Following these three subtests, a numerical comparison is made to compare neck neutral versus neck turned performance. This is known in the literature as the SPNT difference (or SPNTdiff). With the SPNTdiff, we can see if the patient performs differently when their head is straight facing the stimulus or when their neck is turned.
The SPNTdiff = Gain neutral – (Gain neck torsion L + Gain neck torsion R)/2
Note: This equation averages the performance of both neck turned conditions, so you are not able to see in the SPNTdiff which side (neck turned condition) is impacting the results. The SPNTdiff number is reported in the software by the:
- Direction of the stimulus: Left cycles versus right cycles
- Frequency of the stimulus: Speed, 0.1 to 0.5 Hz
- Gain of the eye movement: Right eye = red, left eye = blue
Interpreting results
When comparing neck neutral to neck turned conditions, there are four main parameters to evaluate.
1. Gain of the eye movement
One is gain of the eye movement, which we use to determine how closely the eye is following the target. We can evaluate gain by looking at the individual test graphs. The closer to 100%, the closer the eye followed the target.
See in this example below (Figure 4), the patient had close to 100% gain across most frequencies and in both directions. The only exception is at .1 Hz in the leftward cycle, where they performed at a 75% gain, which was still considered normal for the age of this patient.
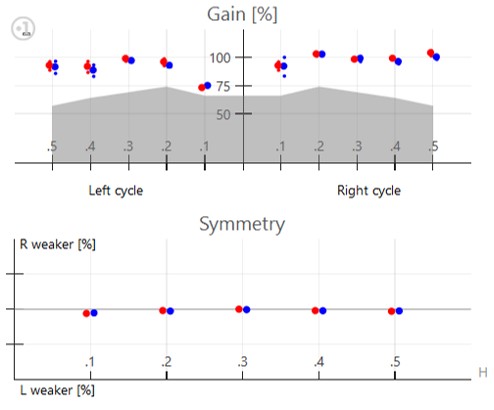
2. Symmetry
The second parameter to look at is symmetry. The symmetry of the recording refers to the direction of the stimulus. Did the patient perform the same when following the dot to the left versus the right or was there a significant difference?
In the example above, you can see the patient performed relatively symmetrically. There is a slight left weakness at .1 Hz due to the slightly lower gain we have already discussed, but nothing is clinically abnormal.
The red dot shows the performance of the right eye, and the blue dot shows the performance of the left eye. Some clinicians also evaluate the congruent nature of the eyes – do they move together when following a target?
3. Quality of the pursuit eye movement
The last parameter we evaluate is not available in a clinical graph but more in the quality of the pursuit eye movement. We look for the presence of saccadic intrusions, such as square wave jerks, macro saccades, and ocular flutter/opsoclonus. These can give us an idea of how smoothly a patient is following the target and likely how clearly they are viewing this stimulus.
It is recommended that before making a statement on the quality of the eye movement, you clean up any noticeable blinks or poor tracking. Be cautious that poor tracking of the pupil is more likely to occur in patients wearing eye makeup.
Note: As with other tests in our battery that assess performance at multiple frequencies, you should look for a pattern of performance. If a patient performs poorly at a lower speed/frequency, you should expect that they will also perform poorly at a higher speed/frequency. This is why it is recommended to look for patterns of performance.
4. SPNTdiff
While we are used to evaluating gain, symmetry, and quality in our normal smooth pursuit test, the SPNT test offers a new measurement parameter known as the SPNT difference (or SPNTdiff). This number is looking for the difference in pursuit performance when in neck neutral versus neck turned (averaged between the sides) conditions.
Note: There is no normative data thus far to determine what is a normal SPNTdiff or what is clinically significant. At this point in the research, the results of the SPNTdiff should alert you of possible cervical contribution to the patient’s symptoms or performance. It may also help you to direct treatment recommendations or interventions accordingly.
Positive SPNTdiff
If there is a positive number, this means the patient performed better in the neck neutral condition (head and body facing stimulus) than in neck torsion conditions. This may mean that the neck is playing a role in abnormal oculomotor performance.
Negative SPNTdiff
If there is a negative number, this means the patient performed better in the neck torsion conditions than the neck neutral conditions. This may or may not be clinically significant. It could indicate a neck position bias (due to previous injury, muscle tightness or strength), an eye weakness (such as a convergence issue), or a learning effect (patient starts to do better as they understand/focus on the pursuit task).
Large SPNTdiff
The larger the number (negative or positive), the bigger the difference in performance between normal neck neutral pursuit and the neck turned condition. This may indicate that the neck is playing a role in abnormal eye movements.
Small SPNTdiff
If there is a small number (negative or positive), this means the patient performed about the same between the neck neutral and neck turned conditions. This either means they did well in all conditions or poorly in all conditions. It is recommended you look at the individual test gains to determine which is the case for your patient.
Significance of the SPNT test
As the profession continues to more holistically care for our dizzy patients, we need to consider evaluation of our patients in more flexible or unique testing positions. In our daily environments, we rarely have our head facing perfectly facing forward while seated upright as we use our oculomotor system for necessary activities.
More likely, our head and body are in unique positions as we use our eyes for everyday needs. The SPNT test advances the VNG forward to better evaluate patients who may have cervicogenic contributions to their dizziness or other visual complaints. This test may pick up on abnormalities we previously missed in patients and helps us make better recommendations or referrals for our patient’s needs.
References
[1] Tjell, C., & Rosenhall, U. (1998). Smooth pursuit neck torsion test: a specific test for cervical dizziness. The American journal of otology, 19(1), 76–81.
[2] Majcen Rosker, Z., Vodicar, M., & Kristjansson, E. (2021). Inter-Visit Reliability of Smooth Pursuit Neck Torsion Test in Patients with Chronic Neck Pain and Healthy Individuals. Diagnostics (Basel, Switzerland), 11(5), 752.
[3] Majcen Rosker, Z., Vodicar, M., & Kristjansson, E. (2022). Video-oculographic measures of eye movement control in the smooth pursuit neck torsion test can classify idiopathic neck pain patients from healthy individuals: A datamining based diagnostic accuracy study. Musculoskeletal science & practice, 61, 102588.
Presenter

Get priority access to training
Sign up to the Interacoustics Academy newsletter to be the first to hear about our latest updates and get priority access to our online events.
By signing up, I accept to receive newsletter e-mails from Interacoustics. I can withdraw my consent at any time by using the ‘unsubscribe’-function included in each e-mail.
Click here and read our privacy notice, if you want to know more about how we treat and protect your personal data.
