Join the Interacoustics community and receive news about new products, events and much more
Top 7 VisualEyes™ 3.2 features for use in neurological patients
VisualEyes 3.2 represents a significant advancement in the field of neurological diagnostics, offering a suite of powerful tools designed to enhance the accuracy and efficiency of patient assessments.
Below, we’ll explore the top 7 features that make VisualEyes 3.2 an ideal tool for evaluating neurological patients.
1. Normative data for Saccadometry
To help you interpret whether your patient’s Saccadometry results are normal or abnormal, we’ve collaborated with research partners to generate normative data. With VisualEyes 3.2, normative data for ages 18-69 years is now available in the software for reference during testing [1].
2. Pupillometry
We’ve switched the measurement parameter in the Pupil Diameter function from pixels to millimeters, offering more clinically useful information for Pupillometry.
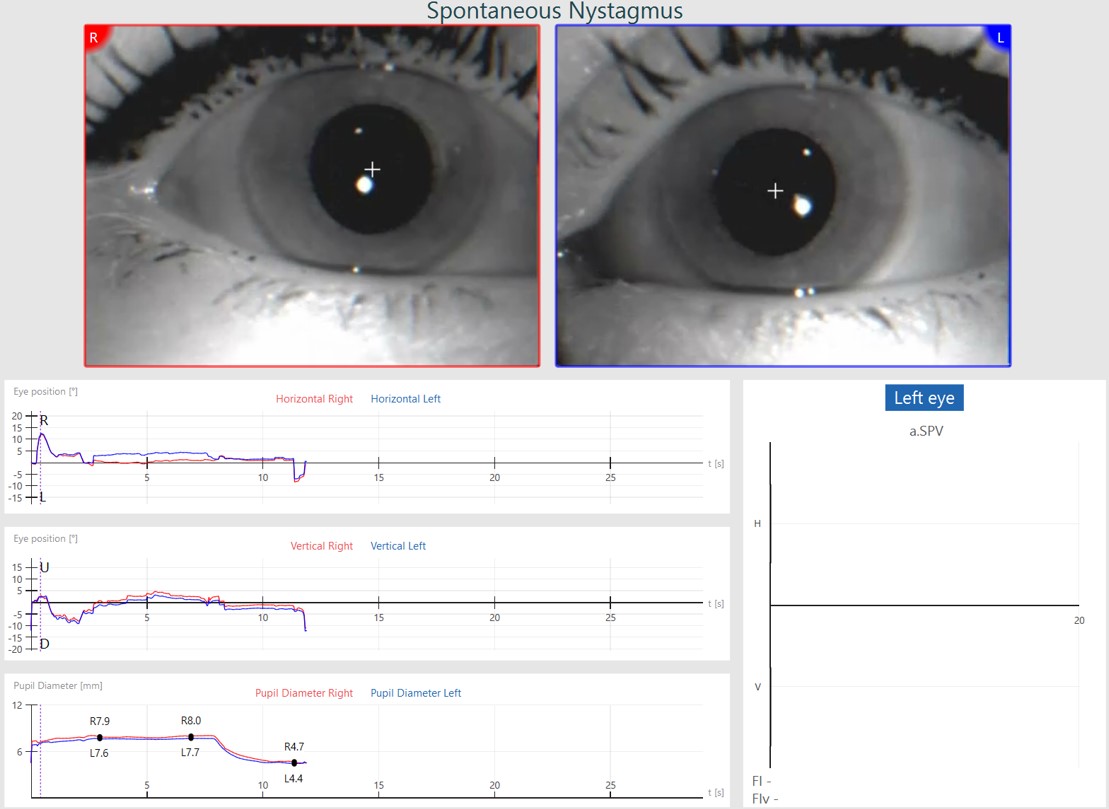
You can also click Edit Tools > ‘+’ sign to add points to the Pupil Diameter graph to get exact measurements of the pupil size at any point during the recording.
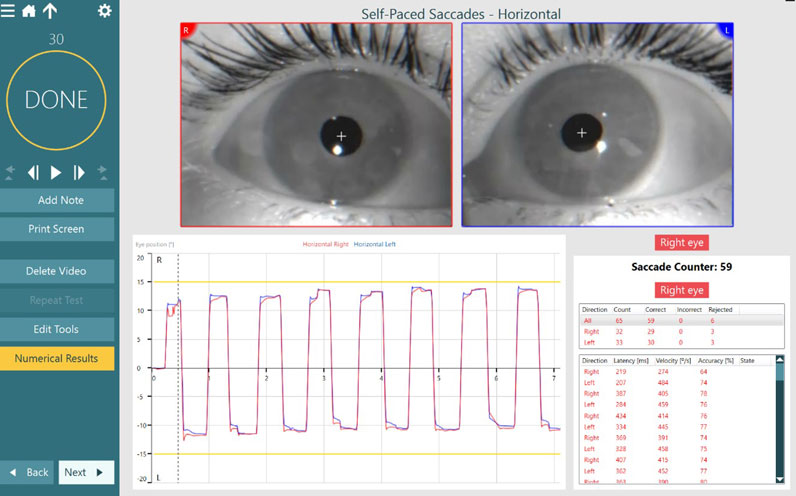
3. Self-Paced Saccades
The Self-Paced Saccade test is an advanced oculomotor task that relies on the patient making voluntary and volitional saccades between two fixed stimulus dots in 30 seconds.
You can perform this test with two horizontal targets or two vertical targets. At the conclusion of testing, similar measurement parameters to Saccade testing are reported: latency, velocity, and accuracy.

There is also a saccade counter present to count the total saccades made during the test. Previous research indicates that patients with central dysfunction, such as a head trauma or neurodegenerative disorder, would have a lower number of total saccades than those without dysfunction. Thus, Self-Paced Saccades can provide extra evidence of central dysfunction.
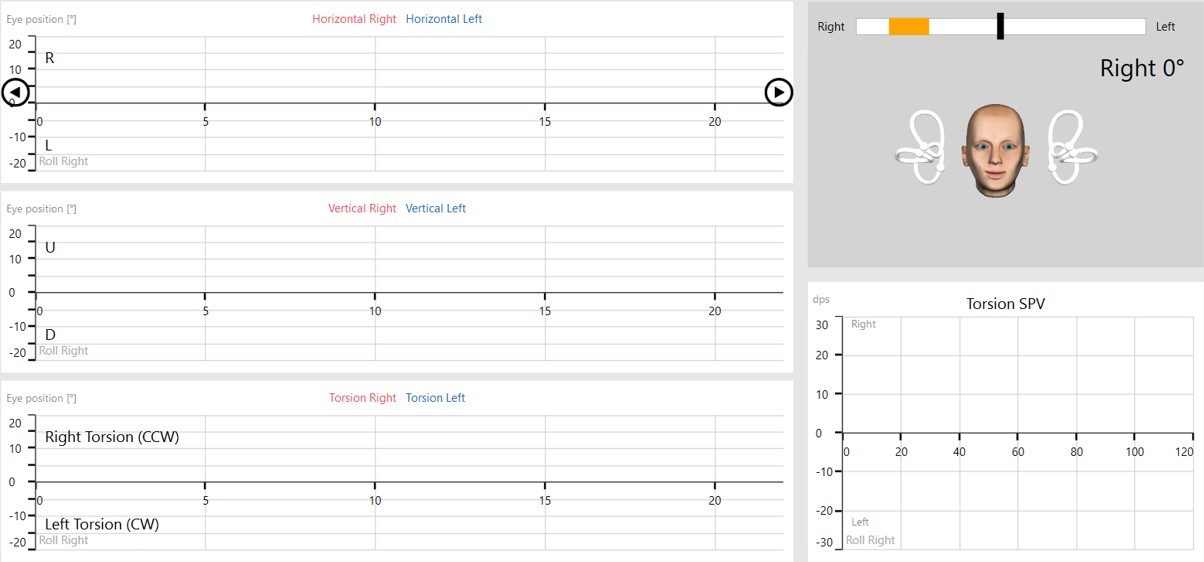
4. Torsion for the Lateral Head Roll test
We have added the torsion eye graph to the Lateral Head Roll test (in VORTEQ Assessments) to better help distinguish between central and peripheral cases.
Read more: Understanding torsional eye movements
5. Cervical-Ocular tests
VisualEyes 3.2 includes two new Cervical-Ocular tests:
Expanding upon the traditional variants of these tests, Cervical Gaze and SPNT testing can help you assess neck contributions to your patient’s performance and symptoms, providing objective data to complement any bedside tests you may be performing.

6. Functional Vision Head Impulse Test (fvHIT™)
fvHIT is a functional assessment of the vestibulo-ocular reflex (VOR) in response to quick head impulses. This test is similar in technique to the Video Head Impulse Test (vHIT), where the patient receives randomized, quick head impulses in each of the canal directions (lateral, LARP, RALP).
However, in the fvHIT test, the patient responds with the direction of the optotype across a broader spectrum of head speed/frequency than what is assessed in the vHIT. We know that vestibular and VOR dysfunction is a spectrum, and fvHIT allows you to see where on the spectrum of function your patient is performing.
7. Ocular Counter Roll (OCR)
The OCR test is not new with VisualEyes 3.2, but is worth mentioning as it is being used increasingly in neurological patients. OCR is a test of otolith function that relies on measuring the torsional shift of the eyes, also known as the ocular tilt reaction (OTR), when tilting the patient’s head 30 degrees toward the right or left shoulder in the roll plane.
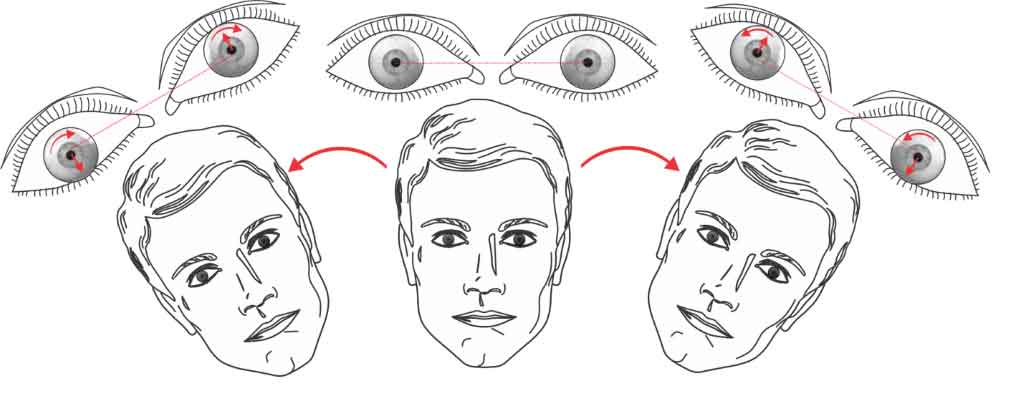
Interpret your OCR findings with caution as both peripheral and central abnormalities are known to affect the OTR. One possible distinction is that central lesions seem to produce disassociated abnormalities in the right and left eyes. Furthermore, the tonic ocular torsion can be either ipsilateral or contralateral to the side of lesion [2].
Advancing the possibilities for evaluating neurological patients
To learn more about how the field of neurology can benefit from Videonystagmography (VNG) and functional VOR testing, please discover VisualEyes 3.2.
References
[1] Demian, D., Petrak, M., Zielinski, G., Massingale, S., Alexander, A., Fuemmeler, L., & Lin, C. C. (2023). Clinical Saccadometry: Establishing Evaluative Standards Using a Simplified Video Oculography Protocol in the Adult Population. Journal of the American Academy of Audiology, 34(1-02), 19–27.
[2] Dieterich, M., & Brandt, T. (2019). Perception of Verticality and Vestibular Disorders of Balance and Falls. Frontiers in neurology, 10, 172.

Similar Topic
Stay up to date!
Subscribe to our newsletter and receive news on new products, seminars and much more.
By signing up, I accept to receive newsletter e-mails from Interacoustics. I can withdraw my consent at any time by using the ‘unsubscribe’-function included in each e-mail.
Click here and read our privacy notice, if you want to know more about how we treat and protect your personal data.
