Subscribe to the Interacoustics Academy newsletter for updates and priority access to online events
Training in VNG
-
Saccadometry in Clinical Practice
-
BSA Guidance for Eye Movement Recordings (2015)
-
BSA Guidance for Positioning Tests (2016)
-
Eye Movements with Progressive Supranuclear Palsy (PSP)
-
Cutoff for Normal vs Abnormal OCR Response
-
Significance of Upbeat Nystagmus in Smokers
-
How Large are Significant Square Wave Jerks?
-
Does Repositioning of Otoconia Affect Utricular Function?
-
How to Differentiate Between Spinocerebellar Ataxia Subtypes Using VNG
-
When is Torsional Nystagmus Significant?
-
Skew Deviation in HINTS Protocol: Next Step?
-
Course: Advances in Videonystagmography (VNG)
-
Course: Advances in BPPV
-
Course: Balance Testing for Beginners
-
Course: Balance Testing for Intermediates
-
What is the Optokinetic Nystagmus Test?
-
What is the Saccade Test?
-
BPPV: Case Studies
-
Benign Paroxysmal Positional Vertigo (BPPV): An Introduction
-
Otolith Testing: Subjective Visual Vertical
-
Otolith Testing: Ocular Counter Roll Test
-
Using the TRV Chair for BPPV Treatment
-
Physiology of the Otolith Organs
-
Diagnosing Central Vestibular Conditions with VNG
-
3D Eye Movement Recordings for BPPV Testing
-
Otolith Testing in VNG
-
The Importance of Vertical and Torsional Eye Movements in the Diagnosis of Vestibular and Neurological Conditions
-
VNG: Gaze Testing Without Fixation
-
VNG: Gaze Testing With Fixation
-
Oculomotor Testing: Theoretical Introduction
-
How to Diagnose Lateral Canal BPPV
-
Course: Saccadometry – a new tool for assessing central vestibular disorders
-
Course: Diagnosing Peripheral Vestibular Disorders
-
Course: The role of repositioning chairs in the diagnosis and treatment of BPPV
-
Course: Which test, when: Exploring optimal vestibular assessment protocol through illustrative case studies
-
Performing calibration for VNG testing
-
Performing spontaneous nystagmus testing (VNG)
-
Performing the gaze test (VNG)
-
Performing smooth pursuit testing (VNG)
-
Performing saccade testing (VNG)
-
Performing optokinetic testing (VNG)
-
Performing Dix Hallpike testing (VNG)
-
Performing positional testing (VNG)
-
Getting started: VNG
-
Understanding torsional eye movements
-
Interpreting the components of protocols that use torsional analysis in VisualEyes™
-
Understanding Jerk Nystagmus
-
The role of eye movements in measuring brain function
-
BPPV: the importance of torsion and performing the manoeuvres accurately
-
Diagnostic driven rehabilitation strategies for concussion and other disorders
-
Physiology of torsional eye movements
-
Measuring torsional eye movements
-
The importance of measuring torsion
-
The role of audiology in concussion diagnostics
-
Eye movements in neuroperformance: A brain focused assessment of eye movements
-
Mise en route: VNG
-
Beyond the basics: Identifying and minimizing artifacts in VNG
-
VPPB: Una Introducción
-
Vidéonystagmographie (VNG) : une introduction
-
Effectuer un test de saccade (VNG)
-
Effectuer le test optocinétique (VNG)
-
Effectuer un test Dix Hallpike (VNG)
-
Effectuer un étalonnage pour les tests VNG
-
Effectuer des tests de position (VNG)
-
Effectuer un test de nystagmus spontané (VNG)
-
Effectuer un test du regard (VNG)
-
Effectuer des tests de poursuite lente (VNG)
-
VNG pruebas oculomotoras
-
Erste Schritte: Video-Nystagmographie (VNG)
-
Kalibration der Augenpositionen
-
Einführung VNG
-
Blickrichtung / Blickstabilisierung Test
-
Spontan Nystagmus
-
Saccaden Test
-
Glatte Blickfolge Test
-
Optokinetik Test
-
Lage-/Lagerungstest
-
Dix-Hallpike Test
-
Kalorik-Test
-
Fundamentos de la VNG: Una vision integral
Interpreting the Dizziness Handicap Inventory (DHI) and VRBQ
Description
Updated by Leigh Martin on April 4, 2023
It’s a very positive step to use these questionnaires alongside the VNG tests to support your diagnosis, guide decision-making, and chart progress of patients.
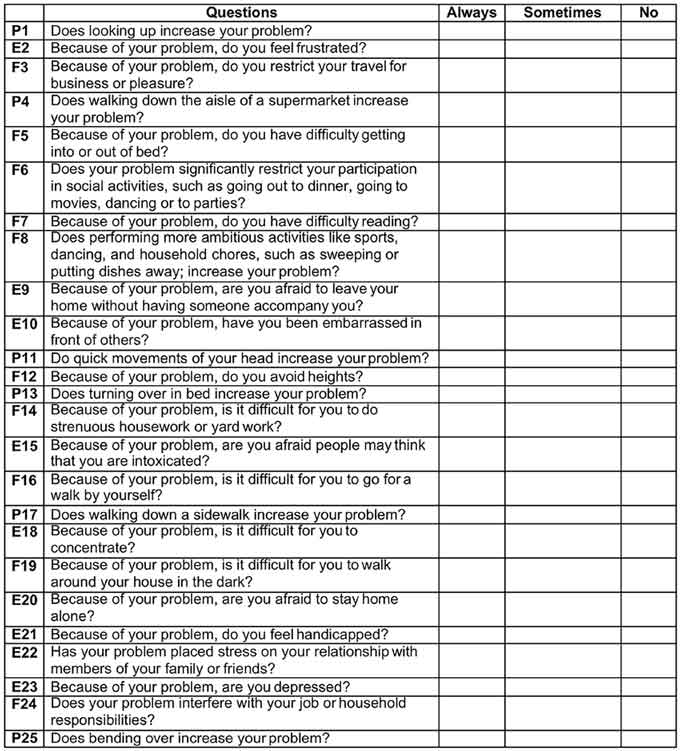
What is the Dizziness Handicap Inventory (DHI)?
The DHI is a 25-question, self-administered questionnaire used to quickly capture the impact of dizziness. The three possible answers to the 25 questions are ‘Always’, ‘Sometimes’, or ‘No’. Always yields 4 points, sometimes yields 2 points, and no yields 0 points. Once completed, the questionnaire gives a total score from 0 to 100 points, which provides an indication of the handicapping effect of dizziness. A score of 0 is no effect, and a score of 100 is maximum effect.
The questions are also grouped into three domains:
- Physical (P)
- Emotional (E)
- Functional (F)
Referring to the responses in each of these domains may help you to gauge the area of most handicap, and thus help to understand where you might place the emphasis in terms of rehabilitation strategies.
See Figure 1 for a complete overview of the DHI.
DHI score change needed to indicate a true change
If you’re using the DHI as an outcome measure to chart progress after a program of vestibular rehabilitation therapy, then you need a change of 18 points in the overall score to consider this a true change.
It’s important to note that the score someone provides on the DHI will not always relate closely with the evidence of peripheral vestibular dysfunction that is indicated by the vestibular test battery. For example, someone may have a high degree of handicap and negative impact on their quality of life, and yet have little or no apparent vestibular dysfunction.
What is the Vestibular Rehabilitation Benefit Questionnaire (VRBQ)?
Like the DHI, the VRBQ provides a snapshot of the overall status at the beginning of a treatment program, which might well be at the point of vestibular assessment. You can repeat it after a vestibular rehabilitation treatment program to assess any changes in the patient’s self-reported status.
The questionnaire has two halves. The first assesses the symptoms, with the responses broken down into three aspects related to:
- Motion
- Anxiety
- Dizziness
The second half assesses the impact of dizziness upon quality of life. The scoring provides a percentage scale, where 0% is no deficit compared with the patient’s own normal state, and 100% is the maximum deficit.
VRBQ score change needed to indicate a true change
You need a change of 7% in the overall score to consider this a true change. You need changes of 6% and 9% to consider these as true changes in the Symptoms and Quality of Life halves, respectively.
Further reading
[1] Jacobson, G.P. and Newman, C.W. (1990) The development of the dizziness handicap inventory. Archives of Otolaryngology Head Neck Surgery, 116 pages 424 - 427.
[2] Morris, A., Lutman, M., and Yardley, L. (2008) Measuring Outcome from Vestibular Rehabilitation, Part I: Qualitative development of a new self-report measure. International Journal of Audiology, 47 pages 169-77.
[3] Morris, A., Lutman, M., and Yardley, L. 2009. Measuring Outcome from Vestibular Rehabilitation, Part II: Refinement and validation of a new self-report measure. International Journal of Audiology, 48 pages 24-37.
Presenter

Get priority access to training
Sign up to the Interacoustics Academy newsletter to be the first to hear about our latest updates and get priority access to our online events.
By signing up, I accept to receive newsletter e-mails from Interacoustics. I can withdraw my consent at any time by using the ‘unsubscribe’-function included in each e-mail.
Click here and read our privacy notice, if you want to know more about how we treat and protect your personal data.
