Subscribe to the Interacoustics Academy newsletter for updates and priority access to online events
Training in ABR
-
Masking in ABR Hearing Testing (1/2)
-
Masking in ABR Hearing Testing (2/2)
-
Rayleigh Medal Lecture 2019 by Dr Elberling
-
eABR: An Introduction
-
CE-Chirp® Research Findings in Infants
-
Tips for Masking Bone Conduction ABR
-
eABR in Cochlear Implantation
-
ABR Case Study: Normal Hearing
-
ABR Case Study: Sensorineural Hearing Loss
-
ABR Case Study: ANSD
-
What is Bayesian Weighting?
-
Course: ABR Correction Factors
-
Threshold ABR for Beginners
-
How to Get Close to Threshold with eABR
-
nHL-to-eHL Correction for ABR Stimuli
-
Why Doesn't Eclipse Have a Notch Filter?
-
ABR Masking Case
-
What is the Binaural Interaction Component?
-
How to Measure Residual Noise
-
Course: Diagnosis and Management of ANSD
-
Course: An Introduction to the CE-Chirp®
-
What is the CE-Chirp® Family of Stimuli?
-
What is Electrode Impedance?
-
90 Hz ASSR or ABR for Threshold Estimation?
-
What is nHL-to-eHL Correction?
-
Cochlear Microphonics for High Frequencies
-
Evoked Responses: What is Wave Reproducibility?
-
ABR: dB nHL vs dB SPL
-
Can Eclipse do Non-Sedated ABR Testing?
-
How to Measure Bone Conduction ABRs
-
2-1-2 and 2-2-2 Toneburst Stimuli Explained
-
What is Auditory Neuropathy Spectrum Disorder?
-
The Role of CE-Chirp® in Newborn Hearing Screening
-
Introduction to the CE-Chirp® Stimuli
-
Demonstration of the CE-Chirp® Stimuli
-
Bone conduction corrections for 500 Hz and 1000 Hz ABR in newborns
-
Bayesian weighting vs traditional artefact rejection in ABR recordings
-
Comparison of 1 kHz and 4 kHz ABR using tone bursts and narrowband CE-Chirp® stimuli
-
CE-Chirp® ABRs in sedated and anaesthetised children
-
Auditory brainstem responses to chirps delivered by different insert earphones
-
Reference hearing threshold levels for CE-Chirp® stimuli
-
ABR using level specific CE-Chirp® stimuli in adults
-
Modelling auditory evoked brainstem responses to transient stimuli
-
Evaluating auditory brainstem responses to different chirp stimuli
-
Auditory brain stem responses evoked by different chirps based on different delay models
-
Development of the CE-Chirp® stimulus
-
Using Fmp and residual noise to stop ABR testing
-
Evaluating residual background noise in auditory brainstem responses
-
The development of Fsp and Fmp
-
The development of Bayesian weighting to recover ABR recordings
-
Noise levels required to mask stimuli used in auditory brainstem response testing
-
Small acoustic tumour detection using ABR and CE-Chirp®
-
CE-Chirp® ABR in normal hearing individuals
-
Improved neural synchronization with the CE-Chirp® stimulus
-
Calculating the residual noise in an ABR waveform
-
Bone Conduction ABR in a Newborn Baby
-
Why Perform Bone Conduction ABR?
-
ABR Testing: Patient Preparation
-
ABR: Testing a Newborn Baby
-
Beyond the Basics: Threshold ABR
-
Two channel bone conduction ABR testing: An interview with Inga Ferm
-
ABR: Testing bone conduction on a newborn baby
-
ASSR vs ABR in children with normal hearing and hearing loss
-
Getting Started: Threshold ABR
-
Las buenas prácticas para realizar un PEATC
-
Umbral PEATC (ABR)
-
Factores de correctión PEATC (ABR)
-
Advances in Pediatric Hearing Assessment
-
La réponse auditive du tronc cérébral (ABR)
Threshold Auditory Brainstem Response (ABR) Testing
Description
Table of contents
- What is the auditory brainstem response (ABR)?
- ABR results interpretation
- Patient preparation
- Testing considerations
- Checking the electrode impedances
- Performing a threshold ABR test
What is the auditory brainstem response (ABR)?
The auditory brainstem response (ABR) is an action potential generated by the brainstem in response to the presentation of an auditory stimulus. The auditory brainstem response is made up of a series of seven peaks and troughs which are generated by neural firing at different – but sometimes overlapping – stages of the pathway (Figure 1).
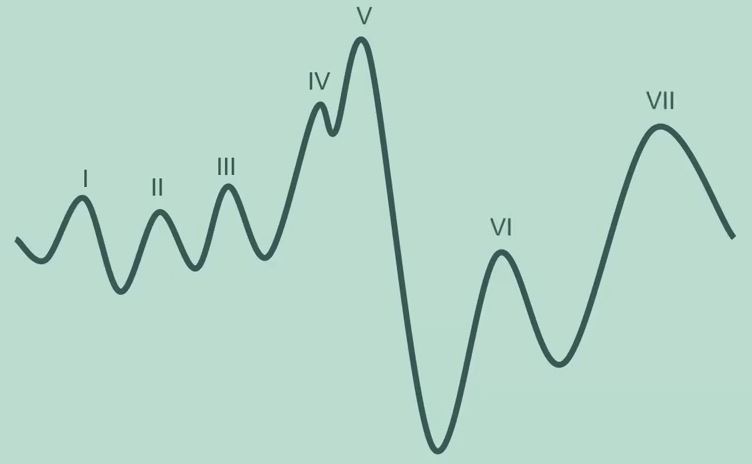
ABR waves
Waves VI and VII are of little clinical utility, leaving waves I-V as those focused on in clinical practice. Wave V is the primary focus of threshold ABR testing being the largest peak and thus easiest to detect.
ABR amplitude
The ABR is unaffected by sleep so can theoretically be recorded when the patient is awake or asleep. However, it is a relatively small evoked potential response. Certainly in comparison to responses generated by the cortical region, which show much larger amplitudes.
Because of the small nature of the ABR amplitude, it can be easily lost within any other noise that may be recorded by the system. This means that testing with an asleep or very settled patient is recommended to ensure good quality recordings can be obtained.
ABR morphology
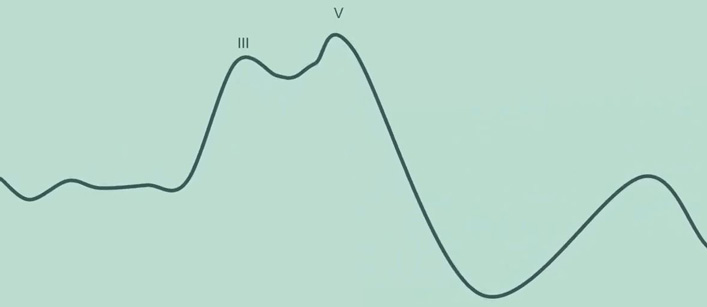
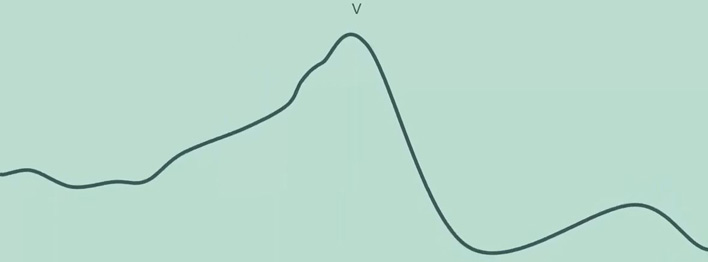
The shape of the ABR is known as the morphology. Figure 1 above is a textbook example but more often than not in clinical practice, the ABR response can look very different to this, and you can expect to see significant variability between patients.
Sometimes only waves III and V can be clearly distinguished within the waveform (Figure 2).
Frequently however, only wave V can be identified (Figure 3).
ABR results interpretation
Depending on:
- Stimulus type
- Frequency
- Intensity level
- Degree and type of hearing loss
Many different ABR morphologies can be recorded, and this can make waveform interpretation challenging for new or inexperienced testers. The key to determining whether an ABR response is present – and thus whether the patient can hear the sound being presented to their ear – is by identifying wave V.
How to identify wave V
There are some fundamental principles that can help in this process.
1. Morphology
Firstly, the morphology of the ABR matters. It should look and feel like an ABR on the screen, particularly the characteristic wave V peak followed by the trough dropping off shortly afterwards. Noisy waveforms can make this harder to see, so good recording conditions are really important to help with waveform interpretation.
2. Latency
The latency or timing of wave V should be roughly around seven to nine milliseconds. There is normative data available in the literature and built in to some evoked potential testing devices. But this isn't always available for every stimulus type and age group.
It is also common to see latency values out of the ordinary in certain types of hearing losses. A conductive hearing loss for instance is likely to present with much longer latencies than normal hearing. It is important to be able to differentiate between a wave V that may not match the normative data and a spike of noise within the waveform.
3. Amplitude
The amplitude of the waveform is taken from the peak of wave V to the trough that immediately follows wave V. The trough is typically present at a latency of 10 milliseconds, but this can be variable. Typically, ABR amplitudes are between 0.1 and 1 microvolt. In some countries, an amplitude of 0.04 microvolts is used as the minimum acceptance criteria for determining if wave V is present.
4. Latency shift
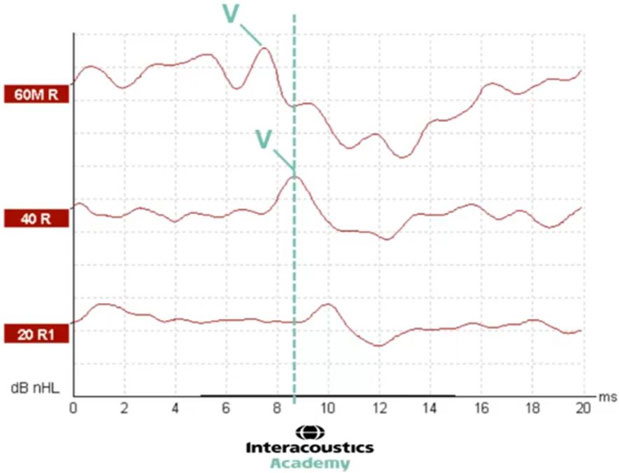
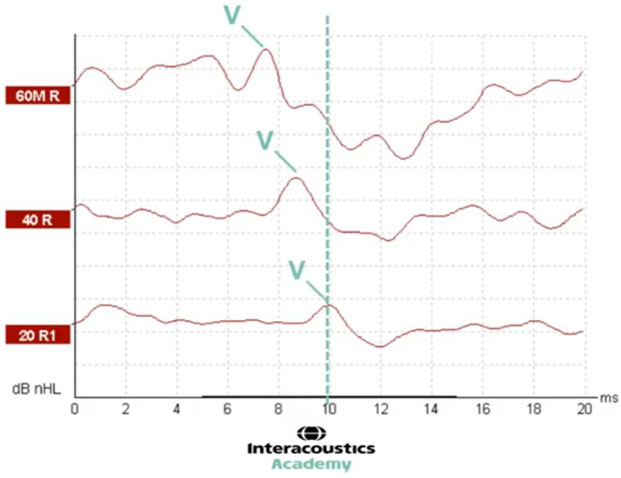
One of the most valuable tools for determining whether a response is present is to look at neighboring intensity levels. An expected pattern of results is to see a latency shift with varying intensity.
Wave V should appear at shorter latencies for louder intensities and at longer latencies for quieter intensities. An amplitude decrease is also expected for quieter intensities and by the same token an increase in amplitude should be seen for louder intensities.
In Figure 4, we have three different intensity levels for the same stimulus. In this instance, the waveforms recorded are good quality with minimal noise and no baseline drift making it easy to identify wave V.
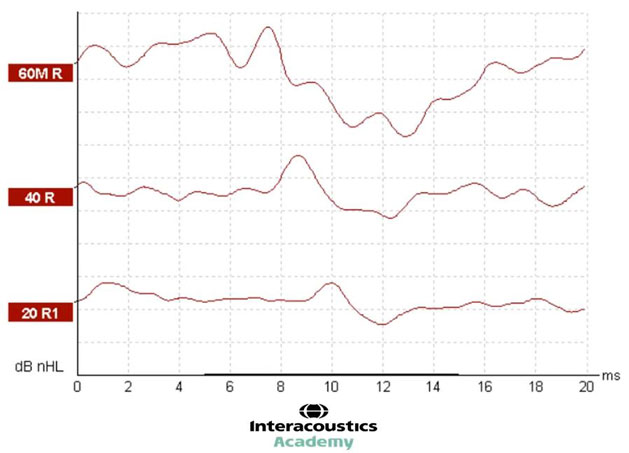
At the level of 60, we can see wave V is present at just before 8 milliseconds. By decreasing the intensity level to 40, we can see that the latency of wave V has shifted to the right. In other words, it is a longer latency. Here, wave V presents at about 8.5 milliseconds (Figure 5).
With a further decrease in intensity, we can see that the latency of wave V has shifted even further to the right, presenting at 10 milliseconds. This demonstrates the expected latency shift as a function of decreasing intensity (Figure 6).
5. Amplitude change
We can also see the amplitude change in this example. At the level of 60, we can highlight wave V and the trough and measure the amplitude as the difference between them (Figure 7).
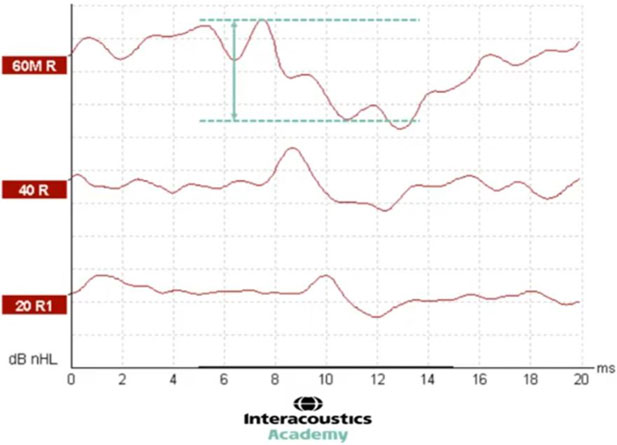
By dropping to a quieter intensity of 40 dB nHL, it is possible to see that the amplitude of this waveform is smaller than that recorded at 60 (Figure 8).
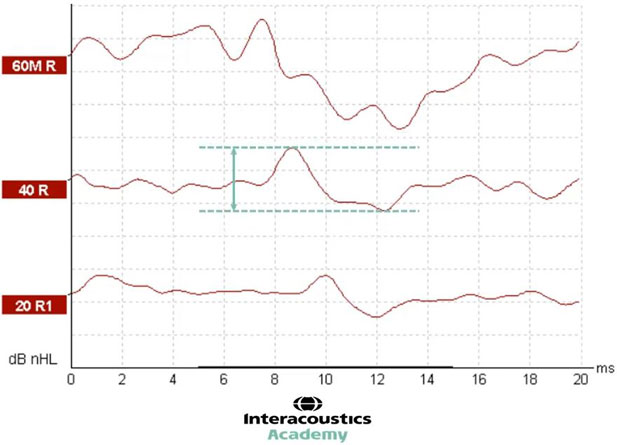
And with a further decrease to 20 dB nHL, the waveform amplitude decreases further yet again (Figure 9).
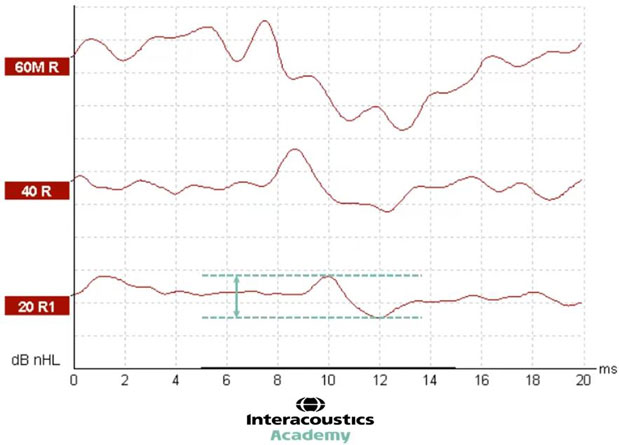
This demonstrates the expected decrease in amplitude when decreasing the intensity level.
By looking for these changes in amplitude and latency, this can help to provide confirmation that wave V has been identified correctly and that the ABR response is behaving as expected. If a set of waveforms do not follow this pattern of results, then further investigation on why is warranted:
- Has there been a technical issue?
- Has wave V been marked incorrectly?
- Do the waveforms contain too much noise?
- Could there be a more complex or unusual type of hearing loss present?
Other tools
There are two objective tools available to assist in determining whether a response is present.
1. FMP
FMP is a statistical calculation provided by the Eclipse software which looks at the likelihood of an ABR being present for newborn babies. A minimum value of 2.2 is recommended by the British Society of Audiology for newborn babies and at least 800 sweeps must be recorded before the FMP value is read.
2. Residual noise
The residual noise within a waveform is also calculated by the Eclipse software. This provides an indication of the quality of the waveform. The lower the residual noise, the better the quality. This can help to guide whether further testing is required to improve the quality of the waveform or whether a sufficiently good quality waveform has been recorded and testing can thus stop. This is particularly valuable when there appears to be no ABR present.
To determine that there is no response, the waveform must be sufficiently lacking in noise to minimize the possibility of a small response being hidden within a noisy waveform. Once the residual noise has reached a suitably low level, the clinician can have confidence that there is minimal noise within which an ABR could be hidden. It is advisable to refer to local guidelines for recommended residual noise stop criteria. However, many clinics use between 15 and 25 nanovolts for newborn babies.
Patient preparation
The following video will demonstrate how to perform skin preparation and electrode placement for ABR testing on a young baby.
Click here to read the full transcript
Preparing the electrode sites
So hi, I'm Amanda and today I'm going to be demonstrating how to perform an auditory brainstem response test. I have a little one-month-old baby with me today. She was born full-time. She's a healthy baby and she's very kindly agreed to do some testing with us today. So we don't want to waste any time, let's get on with getting her ready.
The first thing to do is to prepare the electrode sites. So we have got the Eclipse, which is a two-channel system. So we're going to be using four electrodes today. One on the high forehead, the ground just on the low forehead, and one behind each ear. Those will be our two reference electrodes, and the high forehead will be our active.
So what we need to do is take some electrode gel and a bit of gauze. Or you could use cotton wool. Some people like to use a bit of water or an alcohol wipe before or after doing this. I personally prefer just to use electrode gel. It generally tends to be enough. You don't need much, just a small little blob and we are going to get her high forehead ready.
So you don't need to press hard, it's just about cleaning off any excess oils or dead skin cells. And you don't need to cover a huge area, you just want it to be the area that will be covered by your electrode. So if your baby has a low fontanelle, you do want to avoid that area, so you can go a little bit lower or you can go off to one side. Just be conscious of that when you come to look at your traces.
That looks good. Lovely. We'll just do the low forehead and behind each ear. So on an adult patient, you might be able to put the ground electrode on the low forehead directly underneath your active. But with most babies, you do need to go off to the side because they're so little. Now you can just turn the gauze over and use the dry side just to clean off any of that excess electrode gel.
So with your ear electrode placement, you can either go on the mastoid or on the earlobe. Most babies' earlobes are too little for that option, so we generally go behind the ear on the mastoid. You don't want to be too high up in case you need to do some bone conduction placement later. You also don't want to be too low down so that you're out of the right area.
So you want to get the right balance between doing enough skin preparation so that you don't have to do it again, but not so much that you end up unsettling them and upsetting them so that you can't get them back to sleep again afterwards.
So there is a fine balance between doing enough scrubbing and not too much scrubbing. But hopefully, this will be okay. We'll check our impedances in a moment to see how they are.
Electrode placement
We'll just get these electrodes on. So I'm using these electrodes. I really like these ones, they're nice and sticky. But they also have a bit of conductive gel just in the middle of them. So you don't want to press on that. You want to press on the white bit around the outside. Otherwise, you can make the gel disperse out around.
Testing considerations
Below, we will cover some testing considerations before proceeding with the ABR test.
Making sure the baby is in the right state for testing
As you can see from the previous video, getting the skin prepared for the electrode placement can be a little bit of an upsetting process for the baby. That is why it is worth doing it as soon as possible in an appointment to get that out of the way, then the baby can have a nice little cuddle and settle down.
It is worth sending out some instructions to the parents before they come to the appointment, and it can be a good idea to give them some explanations of what to do and what not to do before they come into the appointment.
For instance, avoiding any moisturizer or oils that morning can be a good idea to help with the skin preparation, but also trying to keep the baby awake as much as possible before the appointment.
Some clinicians recommend having the baby to come in, in a deep sleep so that they're ready to go. However, the risk with this strategy is that when undertaking the skin preparation, that can lift them out of that sleep. It is typically preferable for the baby to come in wide awake and ready to go to sleep, as tired out as possible.
Once the skin preparation is complete, it is a good opportunity to have a little cuddle, have a feed, have a change, whatever the baby needs to do, before proceeding with testing, because we want the baby in as deep a sleep as possible for the auditory brainstem response test.
Where to position the baby?
There's a couple of options for where we position the baby. It's worth talking to the parents and finding out how the baby sleeps best. Are they best in their parent’s arms? In a cot? Do they sleep best on one side or the other?
Ideally, the baby shouldn’t be in the parent’s arms, because there can be interference from the person holding the baby. The ideal situation is to have the baby lying on a neutral pillow or bedding.
That said, the most important requirement of all is a sleeping baby. So, if the baby will not sleep unless they are having a cuddle, or are in their parent’s arms, then that is the best option.
Which ear first?
Clinicians might have an idea as to which ear to start testing based on any previous results, such as newborn hearing screening referrals. However, again, it may be that the baby simply sleeps best on one side or the other, or that they just happen to fall asleep on one side or the other.
Clinicians should be encouraged to go with whichever ear is accessible, unless it is critical to test a particular side first. For instance, if the clinician wanted to test the right ear first, but the baby wouldn't fall asleep unless lying on the right ear, then it can be worth testing the left ear first.
Room environment
A few other considerations before testing are the room setup and the room environment.
Optimal conditions are to have as minimal electrical noise as possible. Mobile phones should be switched off. Any other electrical devices in the room or even those on the other side of the walls on adjacent rooms can sometimes cause some interference.
It is important to know exactly what is set up within and around the testing room. For instance, if a television, microwave, or computer is switched on and it happens to be on the opposite side of the wall that the evoked potentials device is plugged into, then that might cause some interference which could present in the waveforms being recorded.
It is advisable that the room should be acoustically quiet as well.
Checking the electrode impedances
Once your patient is prepared, it's time to connect the electrode cables and check the impedance. If any of the impedances aren't good enough, then you might need to take the electrodes off, re-prepare the skin and maybe put a new electrode on. Usually, the electrode contact does settle over time.
If the impedance check is performed quite soon after placing the electrodes on the skin and the values are slightly higher than desired, then it is worth waiting for a minute or two to see if matters settle down and give the conductive jelly that's inside the electrodes an opportunity to acquire better contact with the skin.
On the Eclipse device, the electrodes are connected to the cable connector that attaches to the preamplifier which in turn is plugged into the Eclipse. Braiding the electrode cables can help eliminate interference.
The ground electrode should be placed either on the low forehead or off to the side (which is commonly required in babies with small foreheads). The vertex is placed on the high forehead, and then the right and left reference electrodes are placed behind each ear.
Once the electrode cables are connected to the electrodes, the impedance check is performed on the preamplifier. Firstly, press the impedance button and then adjust the dial. When the light turns red, that indicates the impedance value for each electrode.
Ideally, all four electrodes should be below 5 kiloohms and balanced so that there is no more than a 2-kiloohm difference between the individual electrodes. If good impedances have not been achieved, it can be worth removing the electrode, re-preparing the skin, and placing a new electrode. However, this should be considered alongside the risk of upsetting and waking the baby up.
If any interference is noted during the test, it is possible to run another impedance check to ensure appropriate impedance values remain. It is also worth running occasional checks throughout the assessment in between waveform acquisitions. After checking impedances, ensure to press the impedance button on the preamplifier to return to testing mode before proceeding with any acquisition.
Performing a threshold ABR test
ABR testing can be performed on adults and children of all ages, and, because the ABR is unaffected by sleep, it is ideal for testing babies who tend to sleep more. When testing older children or adults, sleep is still the ideal state because it reduces the amount of noise that can be introduced to the waveform, but it can be possible to perform the test on an awake patient if they are very calm and settled.
If natural sleep cannot be achieved, it is also possible to perform ABR under sedation or anesthetic without affecting the response.
The next video will show how to perform air conduction ABR testing on an infant with normal hearing.
Click here to read the full transcript
Insertion of transducers
Okay, so now we're ready to start testing, baby's gone nicely to sleep for us, what we do need to do is get some transducers on her ears. Today I'm going to use insert earphones. These are the IP 30 ABR insert earphones. So these are electrically shielded, which helps with again reducing all that possible interference that we might have. As we can see, she's sort of lying on her right side.
So I think we'll try the left ear first, we've got the electrode cables coming away from her. So ideally, we want our insert earphones going the opposite direction to reduce any interference, we don't want these touching. So I'm actually going to spin these around behind me and bring them over here.
Now I've actually cut these little foam insert tips down so that they will fit more easily inside her ears. You can get the silicone ear tips that come in lots of different sizes. I am a big fan of the foam ones just because I find that they grip against the skin a little bit better, but you do need to trim them down a little bit.
So I'm just squeezing that down as flat as possible. We've already looked in her ears earlier, so we're ready to pop this left one in.
Testing strategy and discharge criteria
So, different countries and different hospitals, different clinics will have their own local guidance or national guidance in terms of testing strategy and discharge criteria. So I would always urge you to refer to the guidance for your particular area.
What I am going to do today is work to my discharge criteria, which is ≤ 30 dB HL at 4 kHz in both ears. Now what I want to do is not go straight in at 30 dB HL, I actually am going to start at 10 dB above that discharge criteria so that I can see the growth in the ABR amplitude, and also the shift in latency. That's extra confirmation in terms of looking at waveform morphology.
So for this baby for this age 25 dB nHL is 30 dB eHL. So I'm going to start testing at 35 dB nHL. And we've gone for the left ear because that's the ear that is pointing up, and she seems to be nicely asleep, my EEG is quite calm. Despite little wriggles... we'll just give her a couple of seconds to settle back down again. And I think we're good to start testing.
Left ear 35 dB nHL
As the test continues to run, more sweeps are recorded which contribute to this overall averaged waveform. And we can already see what looks like a typical ABR waveform appearing; we have the characteristic wave V morphology.
Now wave V generally appears at around 7 to 9 milliseconds at this intensity level. But these latencies will vary depending on age and stimulus type and intensity level. In this case, wave V looks like it is emerging at around eight milliseconds. Here we can see the characteristic upward deflection of the wave V, followed by the trough or the SN 10, as some people call it, which typically descends to a point at around 10 milliseconds.
A good quality waveform with little interference or noise will generally be relatively flat throughout the rest of the waveform, allowing for the wave V and the trough to be recognized. If the overall waveform is noisy, or if there's baseline drift, which can lead to a slope to the overall waveform, this can make it much more challenging to pick out the key peaks and troughs.
So it is also useful to make use of neighboring intensity levels, whether these are louder or quieter to look for the shift in latency and amplitude. Now here, we can stop testing the level of 35 nHL. And because we have a clear response, we can move on to testing a quieter intensity.
Left ear 25 dB nHL
So the next level is going to be 25 dB nHL. That gives me my discharge criteria of 30 dB eHL. If I get a response present there, and I've got my 35 dB nHL (which gives me 40 dB eHL) in order to compare the waveforms, look for that growth and that latency shift.
Whilst the waveform for the level of 25 dB nHL starts to average out over time, in order to be as efficient as possible, we can use this testing time to go and start adding waveform markers to the previous level that we've recorded. Now this can become something of a multitasking exercise.
While we are adding markers to the 35 dB nHL waveform, it's important to keep an eye on the level that is currently running, as well as monitoring our patient and the EEG in case we might need to pause testing for any reason. Here, I'm going to add the wave V marker to the 35 dB nHL waveform. I'm going to place that just here.
But now that I'm happy with the morphology of the 25 dB nHL level, I'm actually going to stop testing because we don't need to add any more sweeps. I'm going to add the wave V marker to this waveform, and the trough marker here and also add the trough marker to the 35 dB nHL waveform.
Adding both the wave V and the trough markers allows the software to calculate the amplitude of the waveform. This value is the difference between the peak and the trough, so it's important to add both markers to each waveform.
Edit tab for left ear
Then we can move to the Edit tab within the software, where we can read the precise latency of where we have placed the wave V marker and the amplitude value as well. The software will show the values for the waveform that is selected, so you can switch between them to see these different numbers.
Here, firstly, we can see the values for the level of 35 dB nHL. The latency of wave V is 7.93 milliseconds. And the amplitude from wave V to trough is 0.406 microvolts. We would expect to see a longer latency and smaller amplitude for quieter intensity, and a shorter latency and higher amplitude for louder intensity.
Now we have tested 25 dB nHL which is a quieter intensity. So if we look at the latency value for that waveform, we can see that it is 8.27 milliseconds, which is longer than the 7.93 for 35. And the amplitude for 25 is 0.326 microvolts, which is a smaller amplitude than the 0.406 that was recorded for 35.
So this provides us with the information that confirms the expected latency shift and amplitude change between these two waveforms. And that provides additional confirmation that we have identified wave V correctly in each waveform.
Again, in some countries, they may prefer you to run a repeated level at your discharge criteria just to have that confirmation. Today, I'm not going to do that... I'm going to move on to test the right ear.
Right ear 35 dB nHL
So we need to make sure that we have the right insert earphone in. We need to choose the right ear and again, I'm going to do the same level. So I'm going to start with level 35 dB nHL, that will give me 40 eHL. We're still using a 4 kHz narrowband CE-Chirp, and we're on the right ear now so let's press start.
In addition to eyeballing the waveform morphology, and using the expected latency and amplitude values, as well as the expected latency shift and amplitude change, there is some objective data provided within the Eclipse software that can help inform as to whether there is a response present within the waveform.
The FMP value is a statistical calculation as to the likelihood of a response being present. And it's totally independent of waveform marker placement. However, you must record a minimum of 800 sweeps in order for this calculation to be valid. Typically, in newborns, we're looking for an FMP value of over 7.
In this case, we have recorded over 800 sweeps and our FMP value is over 7 so we can stop testing at any point. Now, we do also have a good morphology, which is further support for the presence of an ABR in this instance.
Right ear 25 dB nHL
Now that we have an ABR recordable at a level of 35 dB nHL, we can go down to test at a lower intensity of 25 dB nHL. While that level is running, I can take the opportunity to mark up the waveform at 35 dB nHL.
If we go back to check on the level of 25 dB nHL that is currently running, we can see a good waveform morphology appearing. Once again we're expecting a latency shift and amplitude decrease compared with the level above and we can see that in this case, now that we are over 800 sweeps, we can read the FMP value, which is also over that critical number of 7, so we can stop testing soon.
Once again, in order to establish the exact latencies and amplitudes for these waveforms on the right ear, we need to make sure that wave V and the trough markers have been placed correctly. Then, we can go to the Edit tab and select each waveform to read these values from the left hand side.
On this Edit page is also where you can see a range of data at the top including the final FMP value, the residual noise and the signal to noise ratio which is calculated based on the waveform amplitude and the residual noise value.
So that is 4 kHz CE-Chirp tested in both ears down to my discharge criteria which is 30 dB eHL in both sides: 25 dB nHL with that +5 correction factor that we need to bear in mind.
Related courses
Presenter

Get priority access to training
Sign up to the Interacoustics Academy newsletter to be the first to hear about our latest updates and get priority access to our online events.
By signing up, I accept to receive newsletter e-mails from Interacoustics. I can withdraw my consent at any time by using the ‘unsubscribe’-function included in each e-mail.
Click here and read our privacy notice, if you want to know more about how we treat and protect your personal data.
