Join the Interacoustics community and receive news about new products, events and much more
What’s new in VisualEyes™ 3.2?
As the vestibular diagnostic world continues to expand beyond Videonystagmography (VNG) testing, new tests and features are becoming a necessity to comprehensively and holistically address dizziness complaints from our patients.
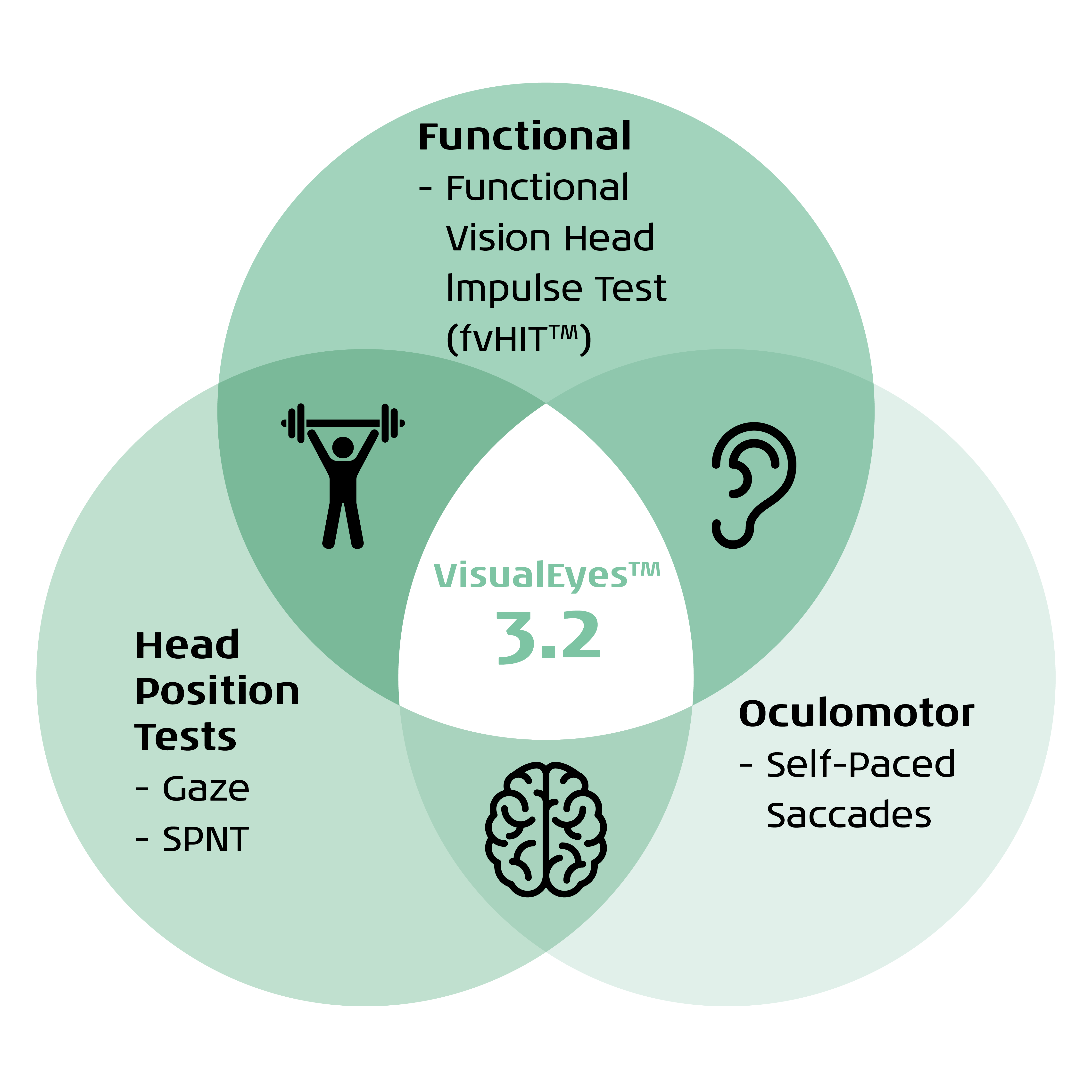
There are several new features releasing in VisualEyes 3.2 that are moving beyond the VNG and bridging the gap between diagnosis and rehabilitation (Figure 1).
Functional Vision Head Impulse Test (fvHIT™)
fvHIT is a functional assessment of the vestibulo-ocular reflex (VOR) in response to quick head impulses. This test is similar in technique to the Video Head Impulse Test (vHIT), where the patient receives randomized, quick head impulses in each of the canal directions (lateral, LARP, RALP).
However, in the fvHIT test, the patient responds with the direction of the optotype. Whereas the vHIT provides objective information on the VOR, the fvHIT provides functional information about how clearly the patient sees in response to quick head impulses. The fvHIT is performed across a broad range of accelerations.

Equipment needed for fvHIT
This test uses the VORTEQ™ IMU head sensor (fixated to the headband in Figure 3) and a remote control. There should also be a smaller monitor to perform the test correctly and accurately. You can perform this test with the VORTEQ Functional Assessments or VORTEQ Assessments bundles.

Clinical utility of fvHIT
The fvHIT test allows for a functional evaluation of the VOR, with a broader spectrum of head speed/frequency evaluated than what is assessed in the vHIT. We know that vestibular and VOR dysfunction is a spectrum, and fvHIT allows us to see where on the spectrum of function the patient is performing. This information can help direct specific therapy and rehabilitation programs to be most beneficial for the patient’s condition.
Self-Paced Saccades
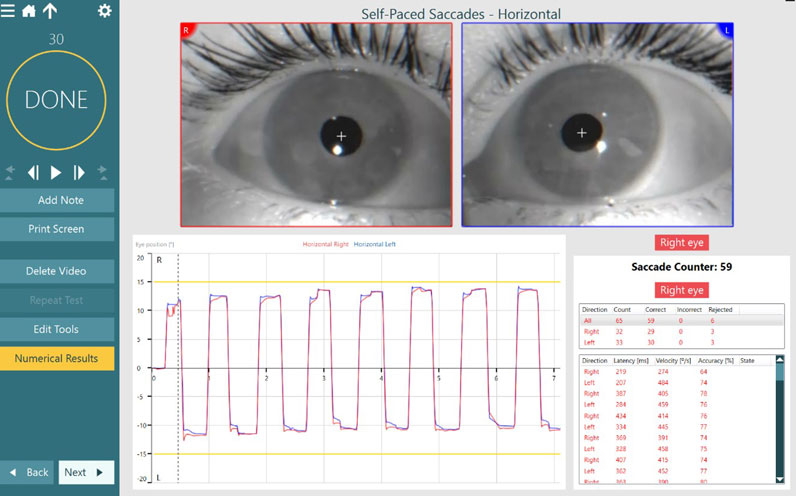
The Self-Paced Saccade test is an advanced oculomotor task that relies on the patient making voluntary and volitional saccades between two fixed stimulus dots in 30 seconds.
You can perform this test with two horizontal targets or two vertical targets. At the conclusion of testing, similar measurement parameters to Saccade testing are reported: latency, velocity, and accuracy.
There is also a saccade counter present to count the total saccades made during the test.

Equipment needed for Self-Paced Saccades
This test uses video goggles and a large stimulus screen to complete the testing. The Self-Paced Saccade test is available as part of VisualEyes 525 and you must turn it on in Protocol Management or add it from Default Tests to include it in your protocol.
Clinical utility of Self-Paced Saccades
Advanced oculomotor tests are finding increased utility in videonystagmography testing due to their sensitivity in identifying dysfunction related to central and neurodegenerative disorders.
Whereas random saccade testing evaluates a patient’s ability to make random, reflexive eye movements towards a target of interest, Self-Paced Saccades rely on volitional initiation of eye movements back and forth between two stationary targets.
Previous research indicates that patients with central dysfunction, such as a head trauma or neurodegenerative disorder, would have a lower number of total saccades than those without dysfunction. Self-Paced Saccades can provide extra evidence of central dysfunction.
Expanded Gaze Positions
We have expanded the Gaze test, allowing clinicians to evaluate eye movements in different head and body positions. Clinicians have always been able to look at eye movements in supine positions; however, we now allow for software- and VORTEQ IMU-guided positioning for seated positions. These tests allow the clinician to determine if the neck is contributing to abnormal eye movements or not.

Equipment needed for expanded gaze testing
This test uses video goggles, a large stimulus screen, and the VORTEQ IMU head sensor. Although you can perform the test without the head sensor, it is most accurate and efficient to perform the test using the sensor. This test is a part of the VisualEyes 525 software bundle.
Clinical utility of gaze testing in different head and body positions
The purpose of this test is to allow the clinician to determine whether the patient’s neck or neck condition is contributing to abnormal eye movements observed during VNG testing.
This ensures that clinical diagnoses can be accurate and recommendations or referrals for treatment are appropriate for that patient’s specific condition.
Smooth Pursuit Neck Torsion (SPNT)
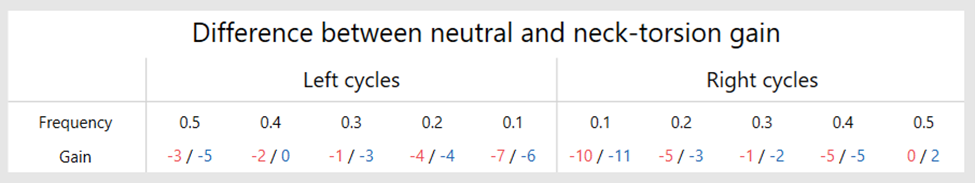
The SPNT test allows for comparison of oculomotor movements in neck neutral versus neck turned conditions. The purpose of this test is to determine if and how much the neck is contributing to abnormal oculomotor performance.
The SPNT test involves three subtests: horizontal smooth pursuit, horizontal body right, and horizontal body left. First, complete the normal smooth pursuit test, and then the neck turned positions.
The comparison of gain between neck neutral and neck turned positions gives us the SPNT difference (SPNTdiff), which is a quantitative measure of cervical influence on oculomotor performance.
Equipment needed for the SPNT test
This test uses video goggles, a large stimulus screen, and the VORTEQ IMU head sensor. Although you can perform the test without the head sensor, it is most accurate and efficient to perform the test using the sensor. The SPNT test is a part of the VisualEyes 525 software bundle.
Clinical utility of the SPNT test
The SPNT test allows clinicians to determine whether the patient’s neck condition is contributing to abnormal eye movements observed during smooth pursuit testing. This information compares neck neutral to neck turned conditions.
If a patient has cervical injury or issues, this test may be an objective evaluation of how the neck may be impacting oculomotor function. If a patient has a higher SPNTdiff number, there is high suspicion that the neck may be a contributing part of abnormal eye movements and/or dizziness.
Deriving this information improves diagnostic accuracy for the patient’s condition, as well as improves opportunities for appropriate referrals to physical therapy for cervical dysfunction.
Move beyond VNG
To learn more about how the world of vestibular is moving beyond VNG, please discover VisualEyes 3.2.

Similar Topic
Stay up to date!
Subscribe to our newsletter and receive news on new products, seminars and much more.
By signing up, I accept to receive newsletter e-mails from Interacoustics. I can withdraw my consent at any time by using the ‘unsubscribe’-function included in each e-mail.
Click here and read our privacy notice, if you want to know more about how we treat and protect your personal data.
