Eclipse Support
Available Training
-
Types of decibels in audiology
-
Tips for the use of Sanibel disposable Tab and Snap electrodes
-
How to Prepare a Baby for Automated ABR
-
Daily System Check
-
IA OAE Suite TEOAE
-
Mounting the Eartip Adaptor
-
IA OAE Suite DPOAE
-
Electrode Tips & Tricks
-
P300/MMN Recording
-
Threshold Testing
-
Neuro Latency Testing
-
Rate Study Protocol
-
Middle Latency Response (MLR)
-
Fmp and Residual Noise
-
How to Improve Evoked Potential Recordings
-
Electrical Auditory Brainstem Response (eABR)
-
Electrocochleography
-
Bayesian Weighting
-
Cochlear Microphonics
-
cVEMP Testing
-
Basic ABR Testing
-
ALR / Cortical Evoked Response Audiometry
-
ASSR Hearing Test
-
How to mark ABR waveforms
-
How to make changes to a saved session
-
How to add a new patient in OtoAccess® Database
-
How to print a report
-
How to customize your ABR protocol
-
How to use the latency tab
-
How to use the recording tab
-
How to use the top panel
-
How to use the edit tab
-
How to navigate the test screen
-
How to prepare the patient for oVEMP testing
-
How to prepare the patient for cVEMP testing
-
How to prepare the patient for ABR and ASSR testing
-
How to prepare the patient for threshold cortical testing
-
How to prepare the patient for ECochG testing
oVEMP Testing
What is the ocular vestibular evoked myogenic potential (oVEMP)?
The ocular vestibular evoked myogenic potential (oVEMP) is an evoked potential measured from the inferior oblique muscle and is used to assess the vestibular system. There is still some debate over the origin of the response (Piker et al., 2011), however, the oVEMP is dependent on the integrity of the superior vestibular nerve (Jacobson et al., 2011).
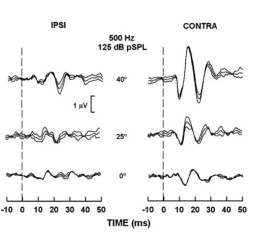
The oVEMP is recorded using surface electrodes at four sites on the face and an Amplitude Asymmetry Ratio is calculated to determine if the above-mentioned parts of the vestibular system are intact and working normally. The figure shows oVEMP recordings from a normal young adult (Murnane & Akin, 2009).
Why oVEMP?
The oVEMP is a test used in addition to traditional vestibular testing (e.g., VNG) to assist in the assessment of vestibular function. oVEMP recordings provide valuable information to medical practitioners to assist them in the diagnosis of disorders such as Superior Semicircular Canal Dehiscence (SSCD) (Watters et al., 2006) and Meniere’s disease (Sandhu, 2012).
How to perform oVEMP testing
Patient preparation is very important. The electrode sites must be prepared and cleaned in order to obtain acceptably low skin impedances. It is recommended to have impedance values of 3kΩ or lower. The impedance value between each electrode should be balanced or similar in value.
The subject is either seated or in a reclined position and is instructed to maintain an upward gaze at 35 degrees for the duration of the recording (Kantner & Gürkov, 2014). Placing a static visual target on the wall or ceiling for the patient to look at during testing will ensure consistent activation of the inferior oblique muscle.
Electrode placement (example)
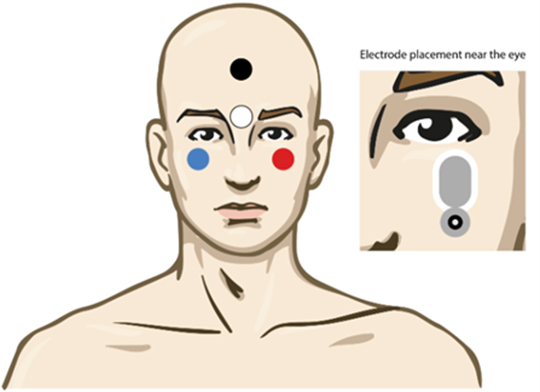

Use of this electrode montage does not require the active (white) electrode to be shifted during testing and is reported to provide large and replicable responses (Sandhu, 2013). Notice the reference electrode is placed slightly laterally from the orbital midline.
The reference electrodes should be placed as close as possible underneath the eye, slightly laterally in the orbital midline. Some clinicians prefer to clip the top part of the electrode to move it even closer to the inferior oblique. Avoid placement close to the medial canthus (inner corner of the eye) as a null-point exists where there is no oVEMP response present (Sandhu, George & Rea, 2013)
The oVEMP response is recorded from the inferior oblique muscle underneath the contralateral eye. Therefore, the right (red) electrode is placed under the left eye while the right ear is stimulated. Correct positioning of the electrode on the inferior oblique muscle is essential in obtaining a response (Sandhu, George & Rea, 2013).
Alternative electrode placements (examples)
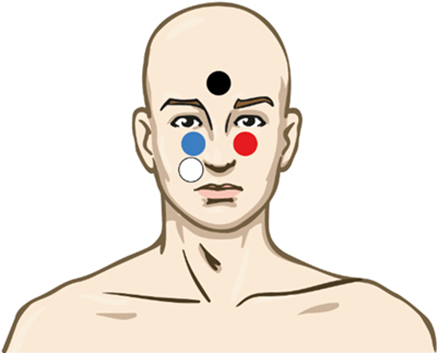
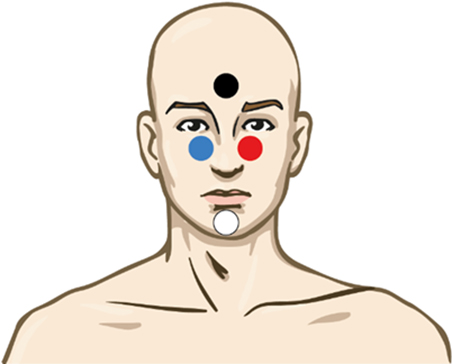
The first figure shows the electrode montage for testing the left ear. For testing of the right ear, move the active (white) electrode to the other side (underneath the red electrode). The second figure shows an alternative electrode montage where no electrodes need to be moved when changing ears.
Typically, the air-conduction stimulus used is a 500Hz tone burst at high intensity level (e.g., 90/95dBnHL). The bone conduction stimulus used is also a 500Hz tone burst at a high intensity level (e.g. 70dBnHL).
Ensure that the patient is relaxed prior to starting the test. After confirming impedances.
Setting up the Eclipse
The Eclipse comes with pre-programmed protocols so the system is ready to use immediately. Protocols can be created or modified easily. Consult the Eclipse Additional Information document to learn how to create or modify a protocol. The procedure described below is simply a suggested test process and to be used only as a guideline.
oVEMP testing procedure
Choose an oVEMP protocol from the dropdown menu 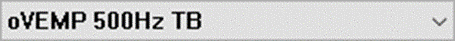
The oVEMP test should be run in the Manual Mode controlling/selecting stimuli manually. For more collection parameters details, please refer to instructions for use manual.
Manual mode
- To begin in manual mode, choose the intensity and select the ear to test on the Record sheet. Instruct the patient to look up and hold their gaze without moving their head.
- Next choose Start or press F2.
- 100-200 sweeps are typically collected per waveform.
Setting up L and R waveform partners
After collection, choose a left or right ear waveform by double clicking the waveform handle. Next, right click the waveform handle of the opposite ear and select Set as VEMP Partner. The selected waveforms are used in the Asymmetry Ratio Calculation.
EMG scaling
The EMG scaling is not to be used in the oVEMP testing, as there is no contracted muscle as in cVEMP. The reason for gazing up, is not to contract the oblique muscle, but instead to position the inferior oblique muscle closer to the recording electrode.
Marking peaks
The oVEMP response is well documented and is said to be represented by two distinct peaks; N1 occurring at approximately 10 ms and P1 occurring at approximately 15 ms.
Waveforms can be marked from the Record sheet or the Edit sheet. To mark a waveform double click on the waveform handle you would like to mark. Right click and then choose the correct marker. Drag your mouse to the correct area and click. You can also choose 1-4 on the keyboard to bring up the appropriate marker and use Enter to place it.
Example of an oVEMP where N1 and P1 are marked for both ears
Normative data
A large study investigating the normal characteristics of the oVEMP by Piker and colleagues (2011) defined an upper limit of oVEMP amplitude asymmetry to be 34% (mean + 2 SD).
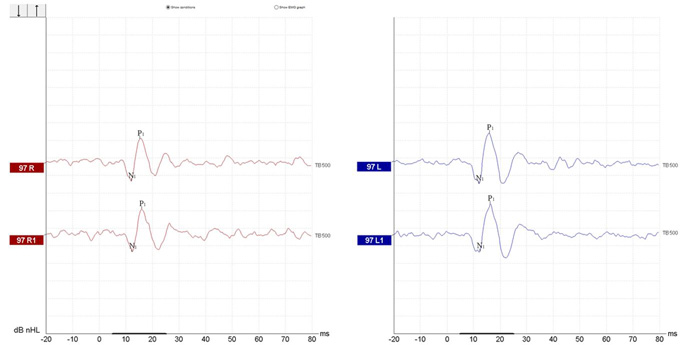
Example of oVEMP waveforms indicating an abnormal asymmetry ratio between left and right side, along with lowered oVEMP thresholds on the right.
Reporting
Choose the Report Icon ![]()
When complete, choose Save and Exit.
References
Kantner, C., Gürkov, R. (2014). The effects of commonly used upward gaze angles on ocular vestibular evoked myogenic potentials. Otology & Neurotology, 35(2), 289-293.
Jacobson, G. P., McCaslin, D. L., Piker, E. G., Gruenwald, J., Grantham, S. L., & Tegel, L. (2011). Patterns of abnormality in cVEMP, oVEMP and caloric tests may provide topological information about vestibular impairment. J Am Acad Audiol, 22,601-611.
Murnane, O. D., & Akin, F. W. (2009). Vestibular-evoked myogenic potentials. Seminars in Hearing, 30(4), 267-280.
Piker, E.G., Jacobson, G.P., McCaslin, D.L., & Hood, L.J. (2011). Normal characteristics of the ocular vestibular evoked myogenic potential. J Am Acad Audiol, 22, 222-230.
Sandhu, J. S., George, S. R., & Rea P. A. (2013). The effect of electrode positioning on the ocular vestibular evoked myogenic potential to air-conducted sound. Clinical Neurophysiology, 124(6), 1232-1236.
Sandhu, J. S., Low, R., Rea, P. A., & Sauders, N. C. (2012). Altered frequency dynamics of cervical and ocular vestibular evoked myogenic potentials in patients with Meniere’s disease. Otology & Neurotology, 33(3), 344-440.
Watters, K. F., Rosowski, J. J, Sauter, T., & Lee, D. J. (2006). Superior semicircular canal dehiscence presenting as postpartum vertigo. Otology & Neurotology, 27(6), 576-768
